What is Shingles?
Shingles (also known as herpes zoster) is a viral infection caused by a reactivation of the varicella-zoster virus (VZV) that causes chickenpox (varicella) (Better Health Channel 2024).
When someone first becomes infected with VZV, they will contract chickenpox. However, after chickenpox resolves, the virus stays dormant in the dorsal root ganglia (nerve cells in the spine) and may reactivate later in life (CDC 2024).
For this reason, only people who have had chickenpox are at risk of shingles (Healthdirect 2023).
Shingles presents as a painful, blistering rash. The reactivated virus generally affects one or two adjacent dermatomes, which are areas of skin that are mostly supplied by a single nerve root branching out from the spinal cord (Oakley 2015; Wiggins & Seervai 2020).
Each of these nerve roots runs from one side of the spine to the anterior middle of the body and sends pain sensations from the dermatome they supply to the brain. For this reason, the rash caused by shingles forms a belt-like pattern on one side of the face or body (chest, back, abdomen or pelvis) without crossing the midline (Better Health Channel 2024; Amin & Yetman 2024).
How Does Shingles Spread?
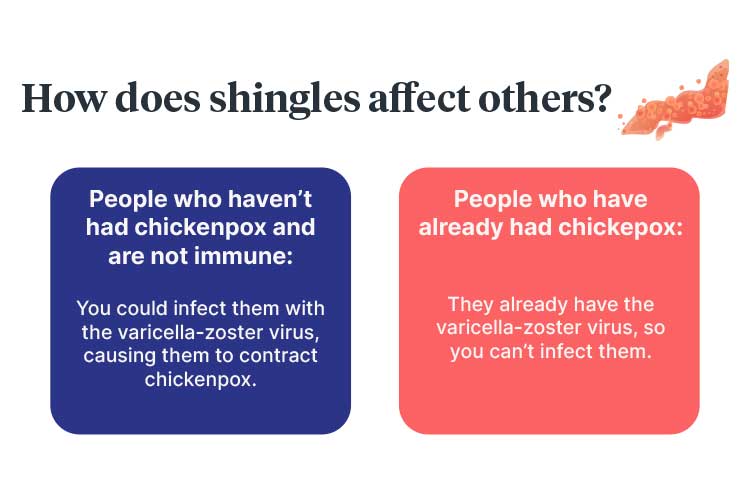
Shingles can only occur after chickenpox - it is not possible to catch shingles from somebody else who has shingles. However, the varicella-zoster virus itself is contagious and can be transmitted through contact with fluid from the blisters caused by shingles (Soliman & Roth 2024).
If a person with shingles transmits VZV to a person who is not immune to the virus, the non-immune person will develop chickenpox. A person who has previously had chickenpox cannot catch VZV from another person as they already have it in their body (Soliman & Roth 2024).
Shingles is much less contagious than chickenpox (VIC DoH 2024).
Risk Factors for Shingles
Anyone who has had chickenpox may develop shingles, but it is most common in people over 50 (Healthdirect 2023). It can occur in children, but this is rare (VIC DoH 2024).
It is estimated that one-third of people will develop shingles during their lifetime (Healthdirect 2023).
There is often no identified trigger for the reactivation of the varicella-zoster virus (Healthdirect 2023). However, known risk factors include:
- Being over the age of 50
- Physical or emotional stress
- Living with human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS)
- Having undergone an organ or bone marrow transplant
- Undergoing treatments for conditions such as cancer that affect the immune system.
(Healthdirect 2023)
Shingles usually only occurs once per lifetime, but some people (especially those who have a weaker immune system) may experience it more than once (Healthdirect 2023).
Shingles Symptoms
The first symptoms of shingles may include:
- Pain in the affected area
- Burning, tingling or itching in the affected area
- Photophobia (light sensitivity)
- Headache
- Fatigue.
(Healthdirect 2023; Better Health Channel 2024)
The characteristic rash generally appears a few days after the onset of these initial symptoms, affecting the area of skin where the discomfort (e.g. burning, tingling or itching) is occurring. It usually persists for 10 to 15 days. During this period, small lesions erupt and form blisters that fill with liquid, burst, and then crust over. This can cause scarring in some cases (Healthdirect 2023; Better Health Channel 2024).

Recovery usually takes two to three weeks in children and young adults, and three to four weeks in older adults (Oakley 2015).
Older adults and those with weakened immune systems are at higher risk of more serious symptoms (AIH 2024).
Complications of Shingles
Shingles usually resolves without issue. However, some people may experience complications such as:
- Post-herpetic neuralgia (pain that persists for more than three months after the shingles rash has resolved)
- Temporary or permanent vision loss caused by shingles in the eye area
- Bacterial infection of the rash
- Pneumonia
- Hearing issues
- Neurological issues such as meningoencephalitis (swelling of the brain) and myelitis
- Ramsay Hunt syndrome.
(Healthdirect 2023; AIH 2024)
Treatment of Shingles
Shingles does not have a cure, but antiviral medicines can alleviate symptoms and reduce the risk of complications. Antivirals are most effective if started within three days of rash onset (Healthdirect 2023).
Other management strategies include:
- Taking over-the-counter paracetamols and non-steroidal anti-inflammatories for pain relief
- Ensuring the rash is kept dry and clean
- Avoiding scratching, as this may aggravate the rash and lead to infection or scarring
- Gently patting the rash dry with a clean towel after showering or bathing
- Wearing loose, cotton clothes in the affected area
- Using cool compresses or taking cool baths
- Avoiding using creams or gels on open blisters.
(Healthdirect 2023; Mayo Clinic 2022)
How is Shingles Prevented?

The risk of developing shingles can be reduced through a vaccination known as Shingrix, which is recommended for all Australians over the age of 50 and given for free to:
- People over the age of 65
- Aboriginal and Torres Strait Islander people over the age of 50
- Immunocompromised people (due to an underlying condition or immunomodulatory/immunosuppressive treatment) aged 18 years and over.
(DoHaAC 2024)
While vaccination does not guarantee protection against shingles, it can reduce the likelihood of its occurrence (Healthdirect 2023).
A second shingles vaccine, Zostavax, is no longer funded under the National Immunisation Program but may still be accessed. However, Zostavax is considered less effective than Shingrix and is a live vaccine, meaning it is contraindicated for immunocompromised people (AIH 2024).
Unlike Zostavax, Shingrix is not a live vaccine (AIH 2024).
The varicella vaccine, which is generally received during childhood, is effective in preventing chickenpox and, subsequently, shingles in 80 to 85% of people (VIC DoH 2024).
People who have shingles should take preventative measures to avoid spreading the varicella-zoster virus to those who are not immune (i.e. those who have not had chickenpox or the chickenpox vaccine). They should:
- Cover the rash with a non-stick dressing
- Refrain from touching or scratching the rash
- Perform frequent hand hygiene
- Refrain from sharing towels, playing contact sports or swimming
- Avoid contact with immunocompromised or vulnerable people, or those who have not had chickenpox or the varicella vaccine.
(Healthdirect 2023; NIA 2021)
The shingles rash is no longer contagious once it has crusted over (Healthdirect 2023).
Test Your Knowledge
Question 1 of 3
A person who has previously had chickenpox is exposed to shingles. What happens next?
Topics
References
- Amin, S & Yetman, D 2024, ‘Does Shingles Follow Nerve Pathways?’, Healthline, 19 March, viewed 13 January 2025, https://www.healthline.com/health/nerve-paths-that-shingles-follow
- Australian Immunisation Handbook 2024, Zoster (Herpes Zoster), Australian Government, viewed 14 January 2025, https://immunisationhandbook.health.gov.au/contents/vaccine-preventable-diseases/zoster-herpes-zoster
- Better Health Channel 2024, Shingles, Victoria State Government, viewed 13 January 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/shingles
- Centers for Disease Control and Prevention 2024, Clinical Overview of Shingles (Herpes Zoster), U.S. Department of Health and Human Services, viewed 13 January 2025, https://www.cdc.gov/shingles/hcp/clinical-overview/
- Department of Health and Aged Care 2024, Shingles (Herpes Zoster) Vaccine, Australian Government, viewed 14 January 2025, https://www.health.gov.au/topics/immunisation/vaccines/shingles-herpes-zoster-immunisation-service
- Healthdirect 2023, Shingles, Australian Government, viewed 13 January 2025, https://www.healthdirect.gov.au/shingles
- Mayo Clinic 2022, Shingles, Mayo Clinic, viewed 14 January 2025, https://www.mayoclinic.org/diseases-conditions/shingles/symptoms-causes/syc-20353054
- National Institute on Aging 2021, Shingles, U.S. Department of Health and Human Services, viewed 14 January 2025, https://www.nia.nih.gov/health/shingles/shingles
- Oakley, A 2015, Herpes Zoster, DermNet NZ, viewed 13 January 2025, https://dermnetnz.org/topics/herpes-zoster/
- Soliman, M & Roth, E 2024, ‘Is Shingles Contagious?’, Healthline, 26 November, viewed 13 January 2025, https://www.healthline.com/health/shingles-contagious
- Victoria Department of Health 2024, Chickenpox and Shingles (Varicella / Herpes Zoster), Victoria State Government, viewed 14 January 2025, https://www.health.vic.gov.au/infectious-diseases/chickenpox-and-shingles-varicella-herpes-zoster
- Wiggins, CJ & Seervai, RNH 2020, Dermatomes, DermNet NZ, viewed 13 January 2025, https://dermnetnz.org/topics/dermatomes/
 New
New