Alarmingly, gonorrhoea cases have doubled over the past 10 years in Australia (Doherty Institute 2024).
With cases on the rise, it’s important to familiarise yourself with the signs and symptoms of this condition.
What is Gonorrhoea?
Gonorrhoea is a sexually transmitted infection caused by the bacterium Neisseria gonorrhoeae (Healthdirect 2024).
Gonorrhoea infection affects the mucosa of the urethra, cervix, rectum, throat and/or eyes, and rarely, the joints, skin or heart (Morris 2023).
What Causes Gonorrhoea?
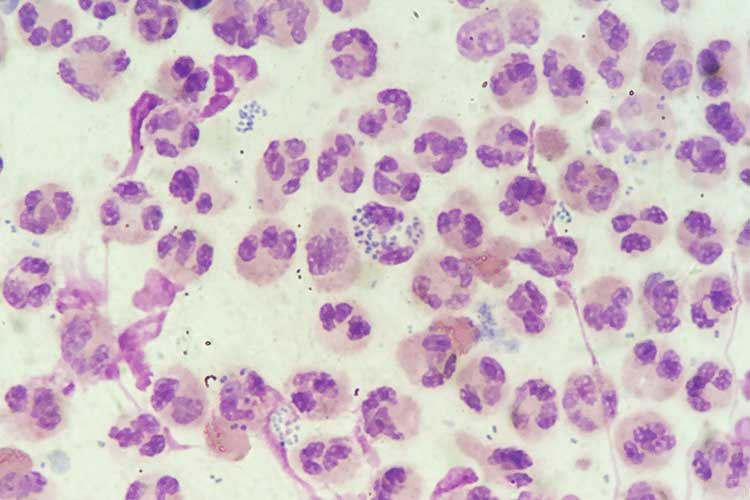
Neisseria gonorrhoeae bacteria are found in penile discharge and vaginal fluid. The infection is spread through unprotected vaginal, oral or anal sex (NHS 2024).
A pregnant person who is infected with gonorrhoea can also spread the disease to their newborn during childbirth when the neonate makes contact with the infected cervical or urethral mucosa. This can lead to gonococcal conjunctivitis, which may cause permanent blindness in the baby (Costumbrado et al. 2022).
Risk Factors for Gonorrhoea
Those at increased risk of contracting gonorrhoea include:
- People who are sexually active, especially if partaking in unprotected sex
- People who inject drugs
- People travelling to areas where gonorrhoea is common
- Aboriginal and Torres Strait Islander people
- Sex workers
- People diagnosed with sexually transmitted infections, including HIV, syphilis and chlamydia.
(Better Health Channel 2020)
Symptoms of Gonorrhoea
The likelihood of experiencing symptoms depends on the area of the body affected:
- Anal and pharyngeal gonorrhoea are almost always asymptomatic
- Vaginal gonorrhoea is asymptomatic in 80% of cases
- Penile gonorrhoea is asymptomatic in 10 to 15% of cases.
(ASHM 2024)
Symptoms, if they do occur, may include:
| Penile symptoms |
|
| Vaginal/cervical symptoms |
|
| Oral symptoms |
|
| Anal symptoms |
|
| Ocular symptoms |
|
(ASHM 2024; Healthdirect 2024; Better Health Channel 2020)
The incubation period is typically two to five days following infection (Healthdirect 2024).
Diagnosing Gonorrhoea

The most effective method of testing for gonorrhoea is via a nucleic acid amplification test (NAAT), which depending on the patient, involves taking an endocervical, vaginal, anorectal or pharyngeal swab, or taking a first pass urine (FPU) sample (ASHM 2024).
A NAAT works by amplifying genetic sequences into millions of copies, allowing even very small amounts of Neisseria gonorrhoeae bacteria to be detected if they are present (Qureshi 2024).
The test can be performed either by a practitioner or at home by the patient (ASHM 2024). It’s likely to be combined with testing for other sexually transmitted infections like chlamydia (Pathology Tests Explained 2024).
Gonorrhoea can also be diagnosed using a gonococcal culture, which allows for antibiotic sensitivity testing. However, this method is less sensitive than a NAAT (ASHM 2024).
Testing can be used to either diagnose active symptoms or screen sexually active individuals (Pathology Tests Explained 2024).
Treatment of Gonorrhoea
Gonorrhoea requires antibiotic treatment and will usually resolve within one week once the regimen has commenced (Better Health Channel 2020).
The first-line treatment for gonorrhoea is both intramuscular ceftriaxone and oral azithromycin. Due to high levels of antibiotic resistance among gonococcal strains, alternatives to this regimen are not recommended except in very specific circumstances (e.g. severe allergy to first-line antibiotics) (ASHM 2024).
The patient should avoid any kind of sexual contact for seven days after the antibiotics are first administered in order to prevent spreading the infection to others. They are also advised to advise their sexual partners that they have gonorrhoea and avoid sexual contact with all sexual partners from the previous two months unless those people have been tested and treated for gonorrhoea (ASHM 2024; Better Health Channel 2020).
Complications of Gonorrhoea
If left untreated, gonorrhoea may lead to serious complications such as:
- Pelvic inflammatory disease (PID), which may scar the fallopian tubes and cause infertility
- Prostatitis, epididymitis or urethral stricture
- Disseminated gonococcal infection (DGI), which occurs when the bacteria enter the bloodstream. This may cause septic arthritis or macular rash
- Bartholin gland abscess
- Meningitis or endocarditis.
(ASHM 2024; Qureshi 2024)
Preventing Gonorrhoea
The risk of contracting gonorrhoea can be reduced by:
- Practising safe sex with condoms and water-based lubricant
- Using dental dams for oral sex
- Getting a full sexual health check annually, including tests for gonorrhoea, syphilis, HIV and chlamydia.
(Healthdirect 2024; Better Health Channel 2020)
Test Your Knowledge
Question 1 of 3
How is gonorrhoea spread from mother to baby?
Topics
References
- Australasian Society for HIV, Viral Hepatitis and Sexual Health Medicine 2024, Australian STI Management Guidelines: Gonorrhoea, ASHM, viewed 27 March 2025, https://sti.guidelines.org.au/sexually-transmissible-infections/gonorrhoea/
- Better Health Channel 2020, Gonorrhoea, Victoria State Government, viewed 27 March 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/gonorrhoea
- Costumbrado, J, Ng, DK & Ghassemzadeh, S 2022, ‘Gonococcal Conjunctivitis’, StatPearls, viewed 27 March 2025, https://www.ncbi.nlm.nih.gov/books/NBK459289/
- Doherty Institute 2024, ‘Research from Pandemic Lockdown Offers Insights Into Gonorrhoea Transmission ’, Doherty Institute News, 23 October, viewed 27 March 2025, https://www.doherty.edu.au/news-events/news/research-from-pandemic-lockdown-offers-insights-into-gonorrhoea
- Healthdirect 2024, Gonorrhoea (The Clap), Australian Government, viewed 27 March 2025, https://www.healthdirect.gov.au/gonorrhoea-the-clap
- Morris, SR 2021, Gonorrhea, MSD Manual, viewed 27 March 2025, https://www.msdmanuals.com/en-au/home/infections/sexually-transmitted-diseases-stds/gonorrhea
- National Health Service 2024, Gonorrhoea, NHS, viewed 27 March 2025, https://www.nhs.uk/conditions/gonorrhoea/
- Pathology Tests Explained 2024, Neisseria Gonorrhoeae Nucleic Acid, Pathology Tests Explained, viewed 27 March 2025, https://pathologytestsexplained.org.au/ptests.php?q=Neisseria+gonorrhoeae+nucleic+acid
- Qureshi, S 2024, Gonorrhea, Medscape, viewed 27 March 2025, https://emedicine.medscape.com/article/218059-overview
 New
New