The kidneys are responsible for filtering waste from the blood and excreting it via urine. However, when the kidneys become damaged, such as in the case of renal failure, they are unable to filter waste properly, causing it to accumulate in the blood (Healthdirect 2024). This is a potentially life-threatening complication (NHS 2021).
What is Dialysis?
Dialysis is a treatment used to artificially filter waste from the blood if the kidneys are no longer able to do so on their own (Healthdirect 2024). While dialysis isn’t a cure for renal failure, it’s a type of supportive care that can sustain the patient until they can receive a kidney transplant, or for the rest of their life if a transplant is contraindicated (NHS 2021).
In the case of acute renal failure, dialysis can be used until the kidneys recover (NHS 2021).
Specifically, the role of dialysis is to:
- Remove waste, salt and excess water from the blood
- Maintain a safe level of electrolytes such as potassium, sodium and bicarbonate in the blood
- Regulate blood pressure.
(NKF 2023)
Dialysis is typically required once a patient enters end-stage renal failure, which occurs when 85 to 90% of kidney function has been lost and their glomerular filtration rate (GFR) is under 15 (NKF 2023).
Types of Dialysis
There are two types of dialysis:
- Haemodialysis
- Peritoneal dialysis.
(Healthdirect 2024)
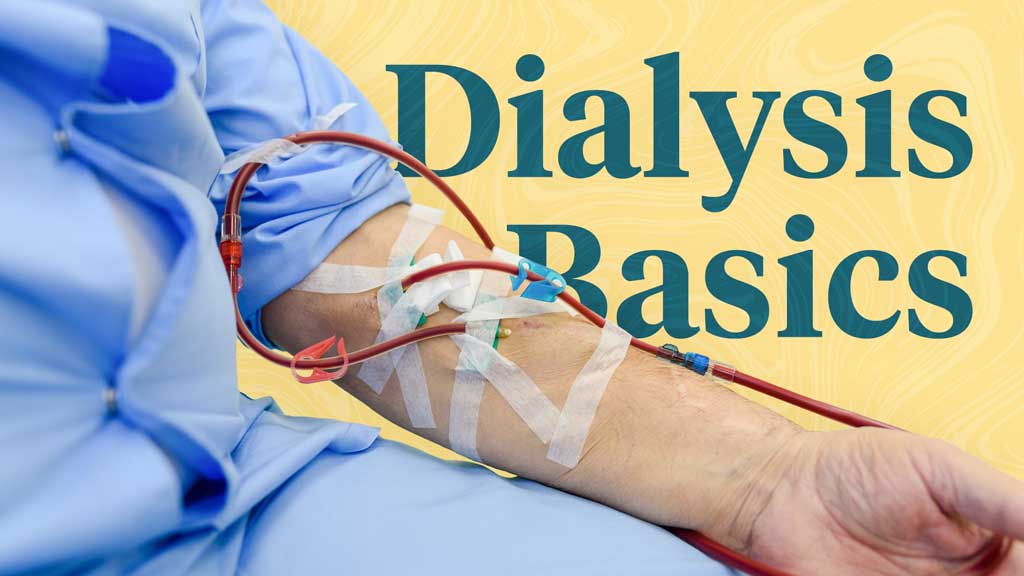
Haemodialysis
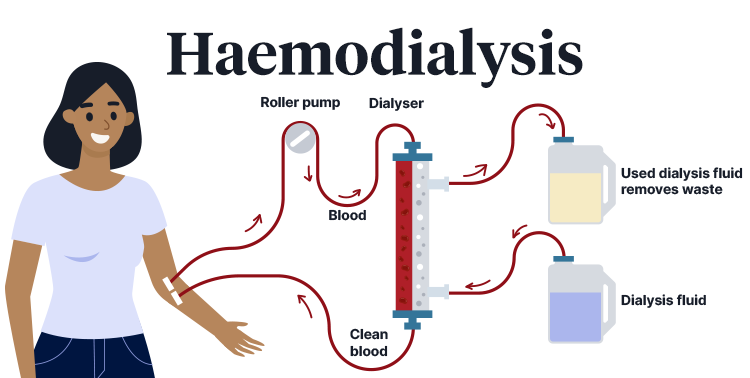
Haemodialysis, which is the most common type of dialysis, involves filtering blood through an external device known as a dialyser (NHS 2021; Healthdirect 2024).
The procedure involves gaining vascular access to the patient’s arm or leg (either via a fistula, graft or catheter) and drawing blood into a tube connected to the dialyser. The blood is then filtered through the dialyser before being circuited back into the patient’s bloodstream. Only a small amount of blood is outside of the patient’s body at one time (Better Health Channel 2022).
The process takes four to five hours and should be performed at least three times per week (Better Health Channel 2022).
Haemodialysis can be performed at a haemodialysis unit or satellite centre or in the patient’s home, provided the appropriate equipment is available (Better Health Channel 2022).
Home haemodialysis is generally preferred as it allows the patient to tailor their treatment schedule to their needs (e.g. while they are sleeping) and receive dialysis more frequently, which will improve their health (Better Health Channel 2022).
Peritoneal Dialysis

Rather than employing an external device, peritoneal dialysis involves using the peritoneal membrane - the lining of the abdominal cavity - as an internal filter (Better Health Channel 2022).
In order to perform peritoneal dialysis, a catheter needs to be inserted into the peritoneal cavity, where it will stay in situ as long as the patient requires dialysis (Better Health Channel 2022).
A cleansing solution (dialysate) is pumped into the body via the catheter, where it absorbs the waste products filtered out of the blood by the peritoneal membrane. The dialysate, now containing the waste, is then drained back out of the body into a bag and replaced with fresh dialysate (Mayo Clinic 2023; NHS 2021).
Each cycle of filling, draining and replacing the peritoneal membrane with dialysate is known as an exchange. There are two different schedules of exchange that may be used:
- Continuous ambulatory peritoneal dialysis (CAPD), where four manual exchanges are performed each day. Each exchange takes about 30 minutes. The process uses gravity - placing the drainage back on the floor drains the fluid out of the body, and raising it above the shoulder allows the new dialysate to flow into the body.
- Automated peritoneal dialysis (APD) involves a machine known as a cycler performing several exchanges overnight while the patient is asleep. The entire process takes 8 to 10 hours, and dialysate is typically left inside the body during the day to continue the dialysis.
(Better Health Channel 2022)
Which Type of Dialysis is Better?
In most cases, both types of dialysis are equally effective and the chosen method will depend on the patient’s preference and lifestyle (NHS 2021).
However, there are certain circumstances where a particular type of dialysis might be preferred:
| Haemodialysis may be preferred for: | Peritoneal dialysis may be preferred for: |
|---|---|
|
|
(NHS 2021)
There are also a variety of pros and cons to consider for each type of dialysis:
| Haemodialysis | Peritoneal dialysis | |
| Pros |
|
|
| Cons |
|
|
(NHS 2021; NKF 2025; NIDDK 2018)
Side Effects of Dialysis
Both types of dialysis can cause side effects. These may include:
Haemodialysis Side Effects
- Fatigue
- Hypotension caused by decreased fluid levels during dialysis
- Nausea or dizziness due to hypotension
- Infection of the vascular access site
- Poor perfusion or obstruction at the vascular access site caused by a blood clot or scar
- Increased risk of sepsis
- Muscle cramps, often in the lower leg - this is believed to be caused by the muscle reaction to fluid loss
- Itchy skin caused by an accumulation of minerals in the body between sessions
- Headache
- Chest or back pain
- Restless legs syndrome
- Sleeping difficulties
- Bone and joint pain
- Reduced libido
- Erectile dysfunction
- Dry mouth
- Anxiety.
Peritoneal Dialysis Side Effects
- Fatigue
- Risk of peritonitis (bacterial infection of the peritoneal membrane), which can occur if the equipment used during dialysis isn’t clean
- Increased risk of hernia
- Weight gain
- Skin infection around the catheter
- Abdominal bloating or discomfort during exchanges.
(NHS 2021; Cleveland Clinic 2021; NIDDK 2018)
Caring For Patients Undergoing Dialysis
Haemodialysis

Patients undergoing haemodialysis should undergo blood testing once per month to ensure that any required adjustments to their dialysis prescription can be made. Furthermore, they should be weighed before and after each treatment and monitor their own weight at home to ensure there is no accumulation of fluid between dialysis sessions (Berns 2025).
The vascular access site should also be monitored and cared for in order to prevent complications. Site care should include:
- Washing the site with warm water and soap every day and before dialysis
- Checking for signs of infection daily (e.g. warmth, redness)
- Checking for perfusion on the site daily
- Discouraging the patient from wearing tight clothes or jewellery, carrying heavy items or sleeping on the affected arm, in order to prevent site trauma
- Avoiding taking blood pressure on the affected arm
- Rotating needle sites on the area and applying gentle pressure to manage any bleeding after injection.
(Berns 2025)
Peritoneal Dialysis
Infection is one of the most serious potential complications of peritoneal dialysis. It’s crucial to know when to escalate care. Signs to look out for include:
- Catheter site infection signs
- Redness, firmness, or tenderness
- Pus-like drainage
- Peritonitis signs
- Mild to severe abdominal pain
- Used dialysate fluid with a cloudy appearance
- Fever
- Nausea or diarrhoea.
(Burkart 2025)
Test Your Knowledge
Question 1 of 3
Overall, which type of dialysis is most effective?
Topics
References
- Berns, JS 2025, Patient Education: Hemodialysis (Beyond the Basics), UpToDate, viewed 20 March 2025, https://www.uptodate.com/contents/hemodialysis-beyond-the-basics
- Burkart, JM 2021, Patient Education: Peritoneal Dialysis (Beyond the Basics), UpToDate, viewed 20 March 2025, https://www.uptodate.com/contents/peritoneal-dialysis-beyond-the-basics
- Better Health Channel 2022, Kidneys - Dialysis and Transplant, Victoria State Government, viewed 20 March 2025, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/kidneys-dialysis-and-transplant
- Cleveland Clinic 2021, Dialysis, Cleveland Clinic, viewed 20 March 2025, https://my.clevelandclinic.org/health/treatments/14618-dialysis
- Healthdirect 2024, Dialysis, Healthdirect, viewed 20 March 2025, https://www.healthdirect.gov.au/dialysis
- Mayo Clinic 2023, Peritoneal Dialysis, Mayo Clinic, viewed 20 March 2025, https://www.mayoclinic.org/tests-procedures/peritoneal-dialysis/about/pac-20384725
- National Health Service 2021, Dialysis, NHS, viewed 20 March 2025, https://www.nhs.uk/conditions/dialysis/
- National Institute of Diabetes and Digestive and Kidney Diseases 2018, Hemodialysis, National Institutes of Health, viewed 20 March 2025, https://www.niddk.nih.gov/health-information/kidney-disease/kidney-failure/hemodialysis
- National Kidney Foundation 2023, Dialysis, NKF, viewed 20 March 2025, https://www.kidney.org/atoz/content/dialysisinfo
- National Kidney Foundation 2025, Choosing Dialysis: Which Type is Right For Me?, NKF, viewed 20 March 2025, https://www.kidney.org/atoz/content/choosing-dialysis-which-type-right-me
 New
New