Between 2021 and 2022, 5,500 Australians were admitted to hospitals for thermal injuries and 120 deaths were caused by thermal injuries (AIHW 2023).
Appropriately managing burns and scalds is essential for all healthcare professionals, particularly those involved in emergency and prehospital care and those working with older people.
What are Burns and Scalds?
A burn is an injury in which the skin or other organic tissue is damaged by heat, radiation, radioactivity, electricity, friction or chemicals (ANZCOR 2023).
A scald is a burn injury caused by a wet agent such as hot water or steam (NHS 2022).
Burns and scalds can vary in severity from minor to potentially fatal, depending on their size and depth (Healthdirect 2023).
What are the Most Common Causes of Burns?
- Hot water
- Heaters
- Oven doors
- Frying pans
- Hair straightener irons
- Fireplaces
- Hot water bottles
- Candle wax
- Hot drinks.
(St John Ambulance Australia (VIC) 2023)
Types of Burns and Scalds
- Thermal burns and scalds are caused by external heat sources such as flames, hot metals, hot liquids, and steam. These sources increase the temperature of the skin tissue, leading to cell death or charring.
- Electrical burns are caused by contact with an alternating or direct electrical current. They include lightning strikes.
- Radiation burns are caused by exposure to ultraviolet radiation from the sun, lasers, nuclear radiation, X-rays and other types of radiation.
- Chemical burns occur when the skin and/or eyes come into contact with hazardous substances.
(Stanford Health Care 2017; ANZCOR 2023)
Acute management will depend on the type of burn being treated.
Burn and Scald Classification
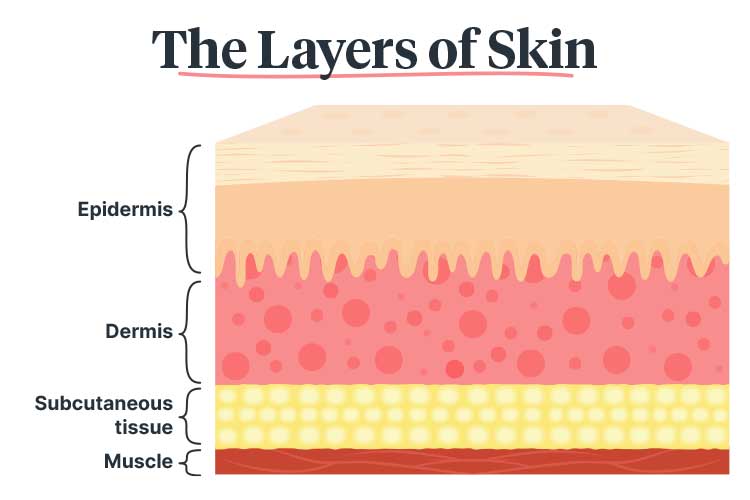
Burns and scalds are classified into one of five categories depending on their depth. They are:
| Category | Depth | Description | Treatment | Image |
|---|---|---|---|---|
| Epidermal | Superficial |
|
|
 (www.vicburns.org.au The Victorian Adult Burns Service, Alfred Health, Melbourne, Australia) |
| Superficial dermal | Partial thickness |
|
|
 (www.vicburns.org.au The Victorian Adult Burns Service, Alfred Health, Melbourne, Australia) |
| Mid dermal | Partial thickness |
|
|
 (www.vicburns.org.au The Victorian Adult Burns Service, Alfred Health, Melbourne, Australia) |
| Deep dermal | Partial thickness |
|
|
 (www.vicburns.org.au The Victorian Adult Burns Service, Alfred Health, Melbourne, Australia) |
| Full thickness | Full thickness |
|
|
 (www.vicburns.org.au The Victorian Adult Burns Service, Alfred Health, Melbourne, Australia) |
(ACI 2024; Victorian Adult Burns Service 2024; Better Health Channel 2023)
What is a Significant Burn?
According to the Australian and New Zealand Committee on Resuscitation, significant burns are those that:
- Affect more than 10% of the total body surface area (TBSA)
- Affect the face, hands, feet, genitalia, perineum or major joints
- Are full thickness burns that affect more than 5% of the TBSA
- Are electrical or chemical burns
- Are associated with inhalation injury
- Affect the circumference of the limbs or chest
- Are experienced by very young (infants or children) or very old patients
- Are experienced by patients with comorbidities that may complicate treatment, extend recovery time or increase the risk of death
- Are associated with trauma.
(ANZCOR 2023)
What is Total Body Surface Area?
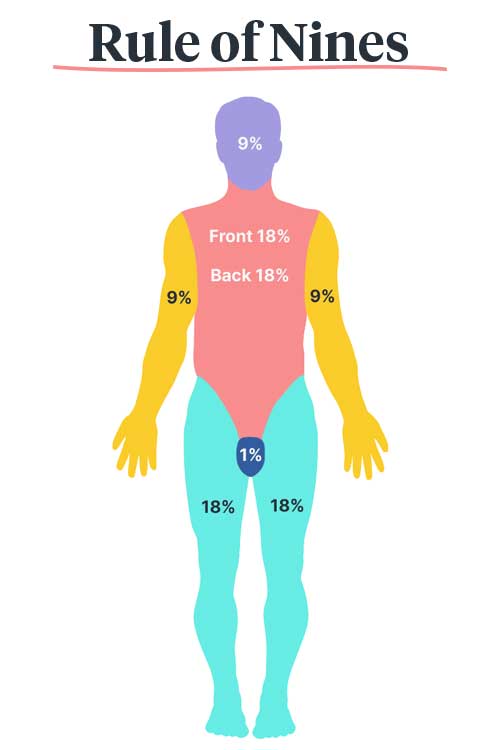
The extent of a burn injury is measured in terms of total body surface area (TBSA). TBSA is calculated using the Rule of Nines, wherein the body is divided into several areas, each representing a multiple of nine (except for the perineum, which is 1%). When all of the areas are added together, they equal 100% of the TBSA (ACI 2024).
Simple erythema should not be included in the TBSA calculation (ACI 2024).
For example, a burn that affects the entirety of a patient’s left arm would be equal to 9% of their TBSA.
Note: Children have different body surface area proportions and therefore require the paediatric Rule of Nines, which differs depending on the child’s age (ACI 2024).
Acute Management of Burns and Scalds
General Management of Burns and Scalds
- Ensure that the patient, rescuers and bystanders are safe.
- Call 000 for an ambulance if the patient has a significant burn or you are unsure whether it is a significant burn (see above for ANZCOR’s definition of a significant burn).
- Avoid entering a burning or toxic atmosphere.
- Stop active burning by:
- Stop, Drop, Cover and Roll
- Smothering flames with a blanket
- Dousing with water if safe to do so.
- Move the patient away from the source of the burning and to a safe environment as soon as possible.
- Assess the patient’s breathing and maintain an open airway. If the patient is not breathing normally, commence CPR (Read: Adult Basic Life Support (BLS) Using DRSABCD).
- Assess for any other injuries if safe to do so.
- Administer oxygen if the patient has smoke inhalation or a facial injury (only if appropriately trained to do so).
(ANZCOR 2023)
Specific steps will depend on what kind of burn the patient is experiencing.
Heat/Thermal/Contact Burns
- Immediately cool the burn with cold running water (between 8 and 25°C, ideally 15°C) for at least 20 minutes (within the first three hours of injury; the sooner, the better). If water is unavailable, a clean, cool liquid such as a soft drink can be used instead.
- You may use commercial cooling gel after 20 minutes of cooling the injury with cold running water, or if cold water is unavailable.
- Remove any rings, watches, jewellery, or other items from the injured area, taking care not to cause further tissue damage.
- Remove any wet non-adherent clothing (as clothes soaked with hot liquids retain heat).
- Cover the injury with a loose, clean non-stick dressing such as plastic cling film. Place the dressing over the injury but do not wrap it around a limb or use it on the face.
- The patient may be at risk of hypothermia. Cover unburnt areas and ensure you keep them warm.
- Elevate burnt limbs to reduce swelling, if possible.
DO NOT:
- Peel off clothing that is stuck to the patient’s skin
- Peel off burnt substances
- Use ice or ice-cold water to cool the burn - this may cause further tissue damage
- Break any blisters
- Use any lotions, ointments, creams or powders.
(ANZCOR 2023; ACI 2024; Victorian Adult Burns Service 2024)
Inhalation Burns
Always assume inhalation burn if the patient:
- Has burns to their face, nose hair, eyebrows or eyelashes
- Has carbon deposits in their nose or mouth.
(ANZCOR 2023)
Other potential indications of inhalation burn are:
- Coughing up black particles in sputum
- Hoarse voice
- Breathing difficulties
- The patient having been trapped in an enclosed area with hot or toxic gas, steam or fumes from a fire or chemicals.
(ANZCOR 2023)
The acute management steps for inhalation burns are:
- Move the patient to fresh air if safe to do so.
- Assess and manage the patient’s airway (Read: Adult Basic Life Support (BLS) Using DRSABCD) Using DRSABCD).
- Administer oxygen if available (only if appropriately trained to do so).
- Call for an ambulance.
Note: Breathing, talking or standing up do not necessarily indicate stability. Delayed pulmonary inflammation may occur up to 24 hours after inhalation.
(ANZCOR 2023)
Electrical Burns
- If possible, isolate or turn off the power supply without touching the patient.
- If high-voltage electrocution has occurred (e.g. fallen power lines), notify emergency services immediately. Stay at least 10 metres away and do not attempt to move wires or objects until the power has been shut off by an authorised person.
- Commence CPR (Read: Adult Basic Life Support (BLS) Using DRSABCD).
- If safe to do so, cool the burn with cold running water. Do this for 20 minutes.
- Administer oxygen if available (only if appropriately trained to do so).
- Call for an ambulance.
(ANZCOR 2023)
Radiation Burns
- Radiation burns should be treated as heat/thermal burns. Note that the patient may display few external signs of injury.
(ANZCOR 2023)
Chemical Burns
Note that the aim of managing a chemical burn is to dilute the agent rather than cool the injury.
- Don appropriate PPE. Do not make contact with the chemical or any contaminated objects.
- Move the patient to safety if safe to do so.
- As soon as possible, remove the chemical and any contaminated clothes or jewellery from the patient. Powdered chemicals should be brushed off the skin.
- Immediately flush the burn with running water. Do this for at least 20 minutes and for up to one hour until stinging has stopped. Avoid spreading the chemical to unaffected areas when doing this.
- If the chemical has entered the patient’s eye:
- Open the affected eye and flush thoroughly with water as long as tolerated.
- If only one eye is injured, the patient’s head should be positioned with the affected eye facing down (so that the chemical does not spread to the other eye).
- Refer the patient for immediate care. However, keep in mind that flushing the eye is more important than immediate transfer for care.
- Call the Poisons Information Centre on 131 126 for treatment advice.
- Check instructions on the chemical container for specific treatment advice.
- Call for an ambulance.
DO NOT:
- Neutralise acid or alkali burns (this increases heat generation and may increase damage)
- Apply cling wrap or hydrogel dressings to chemical burns.
(ANZCOR 2023)
Complications of Burns and Scalds
Burns and scalds may lead to further complications such as:
- Hypovolaemic shock due to fluid loss
- Lung injury from smoke inhalation
- Hypothermia, as burnt skin impairs temperature regulation
- Heat exhaustion or heatstroke
- Loss of consciousness
- Cardiac and/or respiratory distress
- Wound infection, including sepsis in rare cases
- Tissue scarring
- Psychological distress caused by the incident.
(Better Health Channel 2023; NHS 2022)
Preventing Burns and Scalds
Read: Fire Safety in Your Client’s Home
Tips for preventing burns to yourself or your patients include:
- Being cautious when microwaving food and drinks and checking the temperature before serving
- Limiting water temperatures to a maximum of 48.9°C in bathrooms
- Ensuring that nobody smokes near beds or other flammable materials - outside is safest
- Covering unused electrical outlets and keeping electrical cords out of the way
- Ensuring that all smoke detectors work and their batteries are changed regularly
- Donning appropriate PPE if working with chemicals.
(Mayo Clinic 2024)
Test Your Knowledge
Question 1 of 3
Which one of the following scenarios describes a scald injury?
Topics
Further your knowledge
 Free
Free Free
Free
 Free
FreeReferences
- Agency for Clinical Innovation 2024, NSW Burn Transfer Guidelines, New South Wales Government, viewed 30 September 2024, https://aci.health.nsw.gov.au/__data/assets/pdf_file/0004/162634/ACI-Burn-transfer-guidelines.pdf
- Australian and New Zealand Committee on Resuscitation 2023, Guideline 9.1.3 – First Aid for Burns, ANZCOR, viewed 30 September 2024, https://www.anzcor.org/home/first-aid-management-of-injuries/guideline-9-1-3-first-aid-for-burns/
- Australian Institute of Health and Welfare 2023, Injury in Australia: Thermal Causes, Australian Government, viewed 30 September 2024, https://www.aihw.gov.au/reports/injury/thermal-causes
- Better Health Channel 2023, Burns and Scalds, Victoria State Government, viewed 30 September 2024, https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/burns-and-scalds
- Healthdirect 2023, Burns and Scalds, Australian Government, viewed 30 September 2024, https://www.healthdirect.gov.au/burns-and-scalds
- Mayo Clinic 2024, Burns, Mayo Clinic, viewed 30 September 2024, https://www.mayoclinic.org/diseases-conditions/burns/symptoms-causes/syc-20370539
- National Health Service 2022, Burns and Scalds, NHS, viewed 30 September 2024, https://www.nhs.uk/conditions/burns-and-scalds
- Stanford Health Care 2017, Different Types of Burns, Stanford Medicine, viewed 30 September 2024, https://stanfordhealthcare.org/medical-conditions/skin-hair-and-nails/burns/types.html
- St John Ambulance Australia (VIC) 2023, How to Treat and Recognise a Burn - Effective First Aid for Burns, St John Ambulance Australia (VIC), viewed 30 September 2024, https://www.stjohnvic.com.au/news/how-to-treat-and-recognise-a-burn-effective-first-aid-for-burns/
- Victorian Adult Burns Service 2024, Estimate Burn Depth, Alfred Health, viewed 30 September 2024, https://www.vicburns.org.au/wp-content/uploads/2016/06/poster12-different-burn-depth-characteristic.pdf
 New
New