Hospitalised patients with respiratory conditions, particularly those who have undergone chest or abdominal surgery, should perform breathing and coughing exercises in order to prevent further issues and complications (Alberta Health Services 2023).
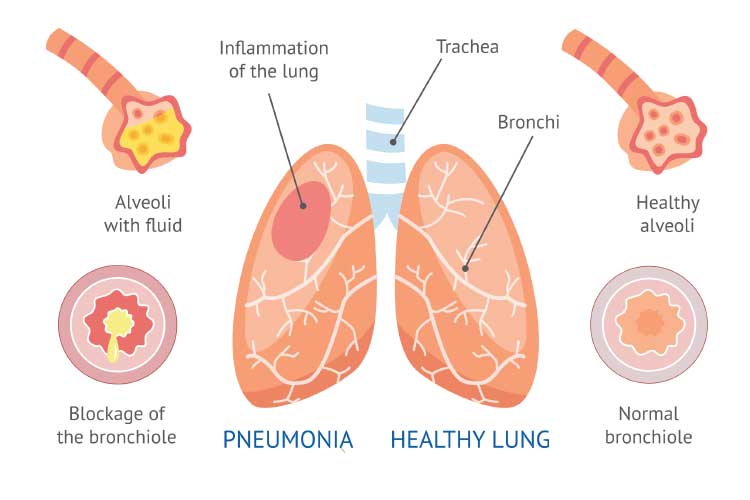
Breathing and coughing exercises are crucial for assisting breathing and clearing excess secretion in the recovery stage. If sputum builds up in the lungs, it may become infected and increase the risk of pneumonia (Alberta Health Services 2023; Penn Medicine 2022).
Furthermore, excess sputum impedes the ability of the lungs to oxygenate effectively (American Lung Association 2025).
A study by the University of Melbourne found that preoperative education and teaching of respiratory exercises halves the rate of post-surgery complications for major abdominal surgery patients (Boden & Denehy 2018).
Which Patients Should Perform Respiratory Exercises?
- Patients with chronic obstructive pulmonary disease (COPD)
- Patients with an interstitial lung disease
- Patients with cystic fibrosis
- Patients undergoing lung, chest or abdominal surgery
- Patients with a muscle-wasting disorder that affects breathing muscles
- Patients with asthma
- Patients undergoing surgery for a lung transplant or lung cancer
- Any patient who may be unable to mobilise.
(MedlinePlus 2018; NHLBI 2022)
What are the Benefits of Respiratory Exercises?
Performing respiratory exercises can help to:
- Strengthen accessory muscles around the lung, as they become weak when a patient is unable to mobilise
- Strengthen the diaphragm, allowing it to assist with lung expansion and improve air reaching the base of the lung
- Take the burden off other muscles in the neck, back and chest that are used when the diaphragm is not working to full capacity
- Clear the airway of excess sputum
- Improve lung function
- Reduce the risk of developing respiratory infections or atelectasis (alveoli collapse).
(American Lung Association 2024; Tokarczyk et al. 2013)
Preparing Patients for Breathing Exercises
- Consider administering analgesia prior to starting. If the patient has pain, they will not be able to perform the exercises.
- Mobilise the patient to ensure they do not acquire a lung infection or atelectasis.
- Sit the patient out of bed or up in bed (the aim is to optimise lung expansion).
- Critical care patients can sit out of bed if they are haemodynamically stable (this allows for better lung expansion). Ensure you have two to three clinicians assisting with any intravenous lines, cardiac monitoring, drain tubes etc.
- Ensure the patient is comfortable.
- Place a folded towel against the patient’s chest or abdomen to provide comfort and security around any wounds.

Types of Breathing and Coughing Exercises
The Active Cycle of Breathing Techniques (ACBT)
The Active Cycle of Breathing Techniques (ACBT) is an exercise comprising three sections:
- Breathing control
- Thoracic expansion exercises
- Huffing (forced expiration technique).
(Bronchiectasis Toolbox 2022)
This technique clears excess sputum and improves lung ventilation. It can be performed in any breath-enhancing position (Bronchiectasis Toolbox 2022).
1. Breathing control
This is a period of relaxed breathing at a rate comfortable for the patient. The patient should breathe in through their nose and out through their nose or mouth until they are ready to progress to the next stage.
(Bronchiectasis Toolbox 2022; Oxford University Hospitals 2024)
2. Thoracic expansion exercises
This exercise aims to mobilise sputum in the lungs.
The patient should breathe in deeply and slowly, through the nose if possible, while trying not to rely on accessory muscles. After holding their breath for 2 to 3 seconds, they should breathe out gently while keeping their shoulders and chest relaxed. This should be repeated up to five times.
(Bronchiectasis Toolbox 2022; Oxford University Hospitals 2024)
3. Huffing
A huff is forceful exhalation of breath with an open throat.
This technique (also known as forced expiration technique) is used to shift sputum from the lower airways to the upper airways so that it can be expelled through the mouth.
The patient should use different lengths of inhalation in order to move the sputum upwards:
- A low-medium volume huff involves taking a small breath in and then huffing. It is used to shift the sputum upwards from the lower airways.
- Once the sputum has moved higher up into the chest, a high-volume huff is then used to move it to the mouth. This involves taking a deep breath in and then huffing.
A rumbling or rattling noise in the chest indicates that the huffing is moving the sputum successfully.
Only one to two huffs should be performed consecutively before another period of breathing control, as they can cause chest tightness or wheezing.
(Bronchiectasis Toolbox 2022; Oxford University Hospitals 2024; ACPRC 2011)
A typical cycle of ACBT comprises:
- Breathing control (until the patient is settled and ready to proceed)
- Chest expansion exercises (three to five)
- Breathing control (until the patient returns to their normal resting breathing rate)
- Chest expansion exercises (three to five)
- Breathing control
- Huffs
- Breathing control.
(Bronchiectasis Toolbox 2022)
This cycle is generally repeated until huffing is no longer producing sputum, or the patient needs to rest (Bronchiectasis Toolbox 2022).

Pursed Lip Breathing
- Relax the neck and shoulder muscles.
- Breathe in through the nose for two seconds.
- Exhale gently through pursed lips for four seconds.
- Repeat as necessary.
(Cleveland Clinic 2023)
Diaphragm Breathing
- The patient should sit up straight and place their hands on their abdomen. Alternatively, the patient can lie down if it is more comfortable for them.
- Take a slow, deep breath in through the nose, ensuring the abdomen expands with the breath.
- Exhale slowly and gently through pursed lips.
- Repeat for 5 to 10 minutes.
(Cleveland Clinic 2022)
Coughing Exercise
- If the patient is lying on their back, they should bend their knees (with permission from their surgeon) and rest their feet on the bed.
- If the patient has undergone surgery, the incision should be supported with their hands or a small pillow.
- The patient should breathe in deeply and cough firmly.
- Clear any sputum into a tissue.
- This should be repeated until the cough is unproductive. However, if the patient has a large amount of sputum, they may need to take a break.
(Alberta Health Services 2023)
Considerations
- The patient may begin to feel dizzy. If this occurs, stop the exercise and observe their vital signs.
- If sputum obstructs the airway, perform basic life support and call for help.
- The patient may experience pain during exercises from surgery or their condition.
- Critical care patients may deteriorate while sitting out of bed due to the sensitive nature of their condition or other complications.
Conclusion
In order to improve lung function and recovery, it is important for the patient to perform breathing and coughing exercises frequently. Patient education is imperative to ensure the exercises are done accurately.
Test Your Knowledge
Question 1 of 3
Which one of the following patients would most likely benefit from respiratory exercises?
Topics
References
- Alberta Health Services 2023, Deep Breathing, Coughing, and Moving After Surgery, Alberta Health Services 2023, viewed 2 May 2025, https://myhealth.alberta.ca/Alberta/Pages/deep-breathing-coughing-after-surgery.aspx
- American Lung Association 2024, Breathing Exercises, American Lung Association, viewed 2 May 2025, https://www.lung.org/lung-health-diseases/wellness/breathing-exercises
- American Lung Association 2025, ‘Understanding Mucus in Your Lungs’, Each Breath Blog, 18 March, viewed 2 May 2025, https://www.lung.org/blog/lungs-mucus
- Association of Chartered Physiotherapists in Respiratory Care 2011, The Active Cycle of Breathing Techniques, Association of Chartered Physiotherapists in Respiratory Care, viewed 2 May 2025, https://www.acprc.org.uk/media/521payl5/gl-05acbt-1.pdf
- Boden, I & Denehy, L 2018, ‘Training for Recovery Before Major Surgery’, Pursuit, 12 March, viewed 2 May 2025, https://pursuit.unimelb.edu.au/articles/training-for-recovery-before-major-surgery
- Bronchiectasis Toolbox 2022, The Active Cycle of Breathing Technique (ACBT), Bronchiectasis Toolbox, viewed 27 April 2023, https://bronchiectasis.com.au/physiotherapy/techniques/the-active-cycle-of-breathing-technique
- Cleveland Clinic 2022, Diaphragmatic Breathing, Cleveland Clinic, viewed 2 May 2025, https://my.clevelandclinic.org/health/articles/9445-diaphragmatic-breathing
- Cleveland Clinic 2023, Pursed Lip Breathing, Cleveland Clinic, viewed 2 May 2025, https://my.clevelandclinic.org/health/treatments/9443-pursed-lip-breathing
- MedlinePlus 2018, Pulmonary Rehabilitation, U.S. Department of Health and Human Services, viewed 2 May 2025, https://medlineplus.gov/pulmonaryrehabilitation.html
- National Heart, Lung, and Blood Institute 2022, Pulmonary Rehabilitation, U.S. Department of Health and Human Services, viewed 2 May 2025, https://www.nhlbi.nih.gov/health-topics/pulmonary-rehabilitation
- Oxford University Hospitals 2024, The Active Cycle of Breathing Techniques, NHS Foundation Trust, viewed 2 May 2025, https://www.ouh.nhs.uk/patient-guide/leaflets/files/96674breathing.pdf
- Penn Medicine 2022, ‘Breathing After Surgery’, Penn Heart and Vascular Blog, 25 May, viewed 2 May 2025, https://www.pennmedicine.org/updates/blogs/heart-and-vascular-blog/2016/october/breathing-and-coughing-after-surgery
- Tokarczyk, AJ, Greenberg, B & Vender, JS 2013, ‘Oxygen Delivery Systems, Inhalation Therapy, and Respiratory Therapy’, in CA Hagberg (ed.), Benumof and Hagberg's Airway Management, 3rd edn, Elsevier, Philadelphia, viewed 2 May 2025, https://clinicalgate.com/oxygen-delivery-systems-inhalation-therapy-and-respiratory-therapy/
 New
New 
