What is Food, Nutrition, and Hydration?
Before diving into the intricacies of a training program, it's crucial to understand the key components. 'Food' involves the solid and liquid substances consumed to provide the body with energy and nutrients. 'Nutrition' deals with the science of how the body uses these nutrients. It's not just about what we eat but also how our bodies absorb and utilise these elements. 'Hydration,' on the other hand, specifically involves maintaining adequate levels of fluid in the body, vital for almost every physiological process.
What is the Food, Nutrition, and Hydration Training Requirement?
According to the Aged Care Quality and Safety Commission and the Australian Commission on Safety and Quality in Health, healthcare providers are required to ensure that their services meet the listed standards. These standards stipulate that the staff must be adept at assessing and maintaining the older persons' nutrition and hydration status, while also fostering an enjoyable quality of life and efficient food and nutrition monitoring systems.
Relevant Standards
Action 5.27: Processes for addressing patients' nutrition and hydration needs
Action 5.28: Food and nutrition systems to ensure:
- Patient nutritional needs are met
- Monitoring of at risk patients' nutritional care
- Patients have access to appropriate nutritional support
National Safety and Quality Health Service (NSQHS) Standards
Requirement 4.3(f): Food provided to clients is to be of suitable quality, quantity and varied.
Action 5.5.4: Maintaining older person's nutrition and hydration
- a. Regularly conducting malnutrition screenings
- b. Minimising chronic conditions on patient life
- c. Responding to patients that are at risk or are malnourished/have experienced unplanned weightloss or gain
- d. Reinforcing access to appropriated health professionals where necessary
Action 6.1.2: Improving food and nutrition monitoring systems
- b. Ensuring patients meet their nutritional requirements
- c. Monitoring health outcomes of older people based on food and drink
- d. Maintaining contemporary evidence-based practice in food and drink.
Action 6.2.1: Assessing client nutrition and hydration
- b. Assessing specific nutritional needs of clients (protein and calcium-rich food focus)
- c & d. When and where the older person likes to eat and drink
- f. Clinical and other physical issues identified that impact the clients ability to eat and drink
Action 6.3.1: Developing and reviewing menus (with clients) to meet their needs
- a. are designed in partnership with older people
- b. are developed with the input of chefs/cooks and an Accredited Practising Dietitian, including for older people with specialised dietary needs
- c. are regularly changed, include variety and enable older people to make choices about what they eat and drink
- d. Enable older people to meet their nutritional needs
- e. are reviewed at least annually through a menu and mealtime assessment by an Accredited Practising Dietitian.
Action 6.3.2: Client choice in food and drink
For each meal, older people can exercise choice about what, when, where and how they eat and drink.
Action 6.3.3: Meals, drinks and snacks provided to older people (including where older people have specialised dietary needs or need support to eat):
- a. are appetising and flavourful
- b. served at the correct temperature and in an appealing way, including the presentation of texture modified foods using tools such as moulds
- c. are prepared and served safely
- d. meet each older person’s assessed nutritional needs
- e. are in accordance with each older person’s choice
- f. reflect the menu.
Action 6.3.4: Food and drink accessibility (at all times)
Older people are offered and able to access nutritious snacks and drinks (including water) at all times.
Strengthened Quality Standards framework analysis - Aged Care Quality Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
Skills Needed for Healthcare Staff to Improve Care through Nutrition
As healthcare professionals aim to offer top-notch patient care, a robust understanding of nutrition and hydration is non-negotiable. While earlier we discussed a variety of skills including menu development, this piece will explore additional competencies required for excelling in nutrition and hydration management. These are crucial across various healthcare settings, including aged care, public and private hospitals, and disability care facilities.
| Skill | Key Elements |
|---|---|
| Knowledge of Nutritional Requirements |
Professionals need a thorough understanding of the dietary requirements for different demographics such as age groups, medical conditions, and even cultural considerations. This knowledge informs proper meal planning and food selection for patients. |
| Fluid Management |
Fluid management is not just about ensuring water intake; it's also about understanding how fluids interact with medications, how they can affect electrolyte balance, and how dehydration can severely compromise a patient's health. |
| Understanding Drug-Nutrient Interactions |
Various medications interact with nutrients in different ways. Healthcare providers need to be aware of these interactions to avoid complications such as nutrient depletion or decreased drug efficacy. |
| Monitoring and Assessment |
Continuously monitoring a patient’s nutritional and hydration status is crucial for early intervention. Healthcare providers should be skilled in techniques like anthropometric measurements, biochemical tests, and clinical assessments. |
| Communication Skills |
Conveying complex nutritional information in an understandable manner to patients and family members is an often-overlooked skill. Good communication is essential for patient compliance and for coordinating with other healthcare professionals. |
How to Assess Staff Competency in Nutrition and Hydration
Ensuring that healthcare staff are competent in documentation is crucial for maintaining high standards of care and legal compliance.
Methods of Assessing Staff Competency in Food and Nutrition
Staff competency can be assessed in the following methods:
- Training and Assessment Framework
Begin by creating a comprehensive training and assessment framework tailored to your specific healthcare environment. This framework will map out the necessary skills and knowledge areas and detail how each will be assessed. - Multiple Assessment Methods
Employ a variety of assessment techniques to ensure a rounded view of staff competencies: written tests, practical assessments, peer reviews, and so forth. - Data Analysis and Tracking
Use data analytics tools to track performance metrics over time. This quantitative approach provides an objective basis for assessment and also helps in identifying trends or areas for focus. - Continuous Feedback Mechanism
Implement regular check-ins and performance reviews focused on food, nutrition, and hydration competencies. These reviews should be constructive, with an aim to foster growth and improvement. - External Audits and Accreditations
External evaluations from governing bodies can also serve as a rigorous check on staff competency. Ensure you meet the relevant criteria set forth by the Aged Care Quality and Safety Commission, or NSQHS.
Strategies to Support Healthcare Staff Improve Nutrition and Hydration Competency
Develop customised training programs that are aligned with your healthcare setting. This would include hands-on training, workshops, and e-learning modules. Using your Learning Management System (LMS) can make tracking and assessment easier.
The following are strategies to improve documentation within healthcare settings:
- Mentorship Programs: A mentorship program can provide staff with an experienced colleague to guide them in real-world scenarios. This offers a two-way learning experience that’s invaluable for skill development.
- Performance Reviews and Feedback Loops Regularly assess employees using key performance indicators (KPIs) directly related to food, nutrition, and hydration. Incorporate 360-degree feedback for a comprehensive review.
- Resource Allocation: Allocate adequate resources, both in terms of materials and time. Staff should be given time during work hours for training and development activities.
- Interdisciplinary Workshops: Interdisciplinary training sessions involving dieticians, physicians, and care staff can offer a holistic view of patient care, emphasising the importance of nutrition and hydration.
- Recognition and Rewards: Incentivising excellence through recognition or tangible rewards can boost morale and encourage a culture of continuous improvement.
- Regular Audits: Periodic internal and external audits can provide valuable insights into the areas that need improvement and also ensure ongoing compliance with national standards.
Sample Training Plan for the Food, Nutrition, and Hydration Training Requirement
Training staff in food, nutrition, and hydration is vital for healthcare organisations. Below is an sample training plan that aligns with Australian standards such as the Aged Care Standards, and NSQHS - based on a mock skills assessment survey.
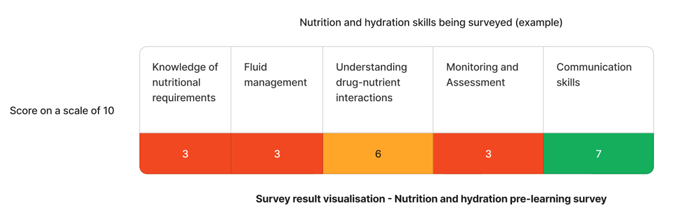
Using the above image as an example - The results that require immediate attention are "knowledge of nutritional requirements", "fluid management", and "monitoring and assessment" skills.
| Quarter | Topics | Resources |
|---|---|---|
| Q1 | Knowledge of nutritional requirements |
|
| Q2 | Fluid management | |
| Q3 | Monitoring and assessment |
|
Need nutrition and hydration training for your staff?
Contact Ausmed today and see how you can enhance your staff's provision of care!
Staff Competency Assessment for Nutrition and Hydration - Example
The following is an example survey that learning and development coordinators may use to asses staff competency on food, nutrition, and hydration.
Staff Survey - Nutrition Competency
-
What are the essential components of a client’s nutritional profile?
[Write your response here]
-
What steps would you take if a client is found to be dehydrated?
[Write your response here]
-
What is the protocol for modifying a client’s dietary plan?
[Write your response here]
-
How do you report food safety issues?
[Write your response here]
-
What methods do you use for monitoring nutritional intake?
[Write your response here]
Conclusion
In conclusion, understanding and implementing effective training and assessment strategies for food, nutrition, and hydration are crucial in healthcare settings. Adherence to Australian healthcare standards is integral in this regard, ensuring both compliance and an enhanced quality of care for patients. Through well-planned training and supportive strategies, healthcare organisations can achieve excellence in this critical aspect of care.
References
- Australian Commission on Safety and Quality in Health, 2023. 'Comprehensive Care Standard'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.27 - Nutrition and hydration'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.28 - Nutrition and hydration'
- Aged Care Quality and Safety Commission, 2023. 'Standard 4. Services and supports for daily living'
- Aged Care Quality and Safety Commission, 2023. 'Stronger Standards, Better Aged Care Program - Action 5.5.4, 6.1.1, 6.1.2, 6.2.1, 6.3.1 - 6.3.4'