Escalating care is essential to patient safety and quality improvement in healthcare. It involves implementing policies and procedures and evidence-based practice to identify and respond to signs of patient deterioration. This proactive approach is integral to maintaining high standards of care when a person is deteriorating. The National Safety and Quality Health Service ( NSQHS) Standards have outlined clear guidelines to ensure all healthcare organisations implement systems and frameworks to maintain patient safety.
What is "Escalating Care"?
Escalating care is defined as a critical process where healthcare professionals can identify signs of deterioration and communicate and get support in a timely manner. The aim is to ensure rapid and appropriate clinical intervention and treatment is administered to prevent further decline.
Why It's Important to Escalate Care
Escalation protocols establish clear, objective guidelines that encourage clinicians to seek assistance when needed. They also support calling for help whenever clinicians, patients, family members, or caregivers have real concerns about a person experiencing acute deterioration (NSQHS). Escalation of care is important in healthcare settings to ensure the patient receives safe and appropriate care. The benefits of escalating care extend beyond patient outcomes; however, they can influence operational efficiency and healthcare team performance.
| Aspect | Benefit | Impact |
|---|---|---|
| Patient Safety | Reduction in adverse events | Improved patient trust and satisfaction |
| Operational Efficiency | Optimised resource allocation | Reduced healthcare costs |
| Staff Performance | Enhanced team communication and collaboration | Increased job satisfaction and reduced burnout |
What is the "Escalating Care" Training Requirement?
Various Australian healthcare standards mandate training for escalating care to equip staff with the necessary skills to act promptly and effectively. The curriculum is designed to address the following:
Relevant Standards
Health service organisation has systems in place with criteria to escalate care, including:
- Agreed parameters (vital signs, and others) of physiological deterioration
- Agreed mental state deterioration indicators
- Agreed parameters and indicators for calling emergency assistance
- When patient pain or distress is not able to be managed using available treatment
- Concern in workforce members, patients, carers, and families about acute deterioration
The health service organisation has processes for patients, families, or carers to directly escalate care
The health service organisation provides the workforce with mechanisms to escalate care and call for emergency assistance
Recognition and response systems to escalate care are used by the workforce.
National Safety and Quality Health Service (NSQHS) Standards
Requirement 3.3 (d): Consumer information:
Change or deterioration (in terms of mental health, cognitive, or physical function or condition)is identified and responded to in a timely manner.
Action 3.2.5: Recognising and responding to client risk and deterioration:
The provider implements strategies to support workers in:
- Recognising risks or concerns related to a client's health, safety and well-being
- Identifying deterioration or changes to older person's ability to perform activities of daily living, mental health, cognitive or physical function, capacity or condition
- Respond to and escalate risks in a timely manner
Strengthened Quality Standards framework analysis - Aged Care Quality Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
What Skills Do Staff Need for Escalating Care?
Effective escalating care requires a multifaceted skill set that enables healthcare professionals to respond swiftly and appropriately to changes in patient conditions. The requisite skills fall into several broad categories, each essential for the rapid recognition and management of clinical deterioration.
- Clinical skills: Ability to perform accurate and timely assessments, interpret clinical data effectively, and recognise signs of deterioration.
- Communication skills: Proficiency in communicating changes in patient condition to the healthcare team, using both verbal and written methods.
- Decision-making: Capacity to make quick, evidence-based decisions regarding patient care.
- Teamwork: Collaborating effectively with the healthcare team to ensure care is coordination is seamless and transparent.
- Knowledge of policies: Understanding of local protocols for escalating care, including knowledge of when and how to engage additional support services.
- Emotional intelligence: Ability to identify and understand the emotional cues of others, during high-stress scenarios.
How to Assess Staff Competency in Escalating Care
Assessing competency in escalating care is a multi-dimensional process that should encompass both theoretical knowledge and practical application. The following methods can be employed to evaluate staff capabilities effectively:
- Direct observation: Supervisors can assess staff during routine clinical duties, noting their ability to identify and react to clinical situations.
- Simulation training: Scenario-based simulations that mimic real-life cases can provide insights into a staff member's response to acute situations.
- Self-assessment: Encouraging self-evaluation can help staff reflect on their own skills and identify areas for improvement.
- Peer feedback: Colleagues can offer valuable perspectives on performance during patient escalation situations.
- Assessments: Written or computer-based testing can gauge a staff member's understanding of the theoretical aspects of patient escalation.
- Performance Reviews: Regular reviews of staff performance, including their ability to escalate care appropriately development.
Strategies to Support Healthcare Staff Develop Skills in Escalating Care
Upskilling staff in escalating care is a continuous process that requires a strategic approach to education and practice. The following strategies can be implemented to foster skill development:
| Strategy | Description | Implementation |
|---|---|---|
| Continuing education | Regular practical training sessions will help staff remain up-to-date and confident in their ability to respond and escalate a deteriorating pateint. The more practical real-life scenario-based learning the better. | Online or in-person training sessions. |
| Mentorship programs | Pair less experienced staff with experienced clinicians . | Scheduled in regular catch-ups and meetings to ensure the individual feels well supported. |
| Simulation | Practical simulations that recreate potential clinical scenarios requiring escalation. | Regularly scheduled simulation exercises, with debriefs to discuss performance and celebrate the wins. |
| Performance feedback | Ongoing constructive feedback on escalating care competencies. | Meet regularly and provide support in areas for improvement. |
Sample Training Plan for the Escalating Care Requirement
The ability of staff to escalate care is extremely important to all aspects of healthcare.
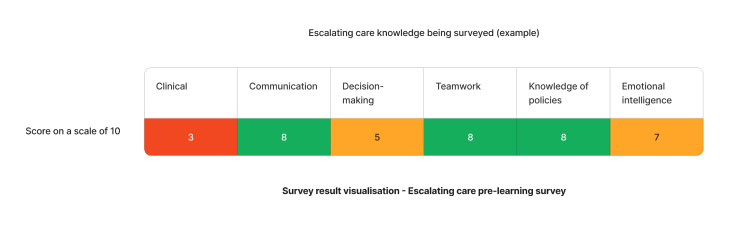
Using the above needs assessment survey as an example - The skill needed for effective escalating care that requires the most attention is clinical. We can target learning initiatives to fill these gaps to enhance staff competency.
Need an LMS that can support care escalation training?
Contact Ausmed today and see how we can support with your care escalation training requirements!
Staff Competency Assessment for Escalating Care - Example
Consider the following survey questions to evaluate care escalation skills:
Staff Survey - Escalating Care Competency
-
Can you describe the steps you would take when you identify a patient exhibiting signs of clinical deterioration?
- [Answer here]
-
How do you communicate and document a change in a patient's condition?
- [Answer here]
-
Explain how you would collaborate with other healthcare professionals during a care escalation scenario.
- [Answer here]
-
Reflect on a past experience where you were involved in escalating care. What were the outcomes, and what did you learn?
- [Answer here]
Conclusion
The implementation of a comprehensive escalating care training program is vital for maintaining patient safety and improving health outcomes. By equipping staff with the necessary skills and knowledge, healthcare organisations can ensure a consistent and effective response to clinical deterioration.
References
- Ede, J, Jeffs, E, Vollam, S, Watkinson, P. A qualitative exploration of escalation of care in the acute ward setting. Nurs Crit Care. 2020; 25: 171–178. https://doi.org/10.1111/nicc.12479
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS - Recognising and Responding to Acute Deterioration Standard'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 8.06'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 8.07'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 8.08'
- Australian Commission on Safety and Quality in Health Care, 2023. 'NSQHS Action 8.09'
- Aged Care Quality and Safety Commission, 2023. 'Standard 3. Personal care and clinical care'
- Aged Care Quality and Safety Commission, 2023. 'Requirement 3.3 (d)'
- Aged Care Quality and Safety Commission, 2023. 'Stronger Standards, Better Aged Care Program - Action 3.2.5'