What is 'End-of-Life Care'?
End-of-life care is the support and medical care provided during the time surrounding death. It involves managing symptoms, ensuring the patient's comfort, and addressing emotional and spiritual needs, both for the patient and their family.
Why is End-of-Life Care Important?
End-of-life care is an increasingly important aspect of healthcare that encompasses medical, emotional, and spiritual support for patients nearing the end of their life. The National Safety and Quality Health Service (NSQHS) Standards, Aged Care Quality Standards, and Strengthened Aged Care Quality Standards have particular actions and clauses focusing on this area (Australian Commission on Safety and Quality in Health Care, 2023; Aged Care Quality and Safety Commission, 2023). This article aims to guide learning and development coordinators and educational managers in establishing an effective training program for end-of-life care.
Is End-of-Life Care and Palliative Care the Same?
Palliative care and end-of-life care are occasionally conflated. Palliative care is a family-centered care provided for an individual with an active, progressive, advanced disease. Palliative can coexist with ongoing treatments for whom the primary goal is to optimise the quality of life. Conversely, end-of-life care, as per the Australian Department of Health and Aged Care (2019), does not entail continued treatment. End-of-life care relies on open communication, informed decision making and collaboration among healthcare providers, families and carers.
What is the 'End-of-Life Care' Training Requirement?
The NSQHS Standards require healthcare services to provide training in the comprehensive care of patients, including those in their end-of-life phase (Actions 5.15-5.20). Similarly, the Aged Care Quality Standards necessitate the delivery of safe, effective personal care, clinical care, or both that is tailored to the consumer’s needs (2.3 b). Lastly, Strengthened Aged Care Quality Standards 5.7.1-5.7.4 specify more rigorous training in this area.
Relevant Standards
Action 5.15: End-of-life care processes
- Processes for end-of-life care align and are consistent with the National Consensus Statement: Essential elements for safe and high-quality end-of-life care
Action 5.16: Access to specialist palliative care advice
- Organisations must create agreements with local palliative care providers to facilitate access to special palliative care advice
- Processes are set up to allow clinicians access to said specialist care advice
Action 5.17: Advance care plan access
- Patients are allowed access to receive said advanced care plans
- Advance care plans are documented in the patient's healthcare record
Action 5.18: Processes in place to support all members of the workforce in providing end-of-life care
Action 5.19: End-of-life care is properly evaluated for safety and quality
Action 5.20: Processes for shared decision making are in place to support clinicians in providing end-of-life care
National Safety and Quality Health Service (NSQHS) Standards
- (b) Assessment and planning is used to identify and addresses the client's current needs, goals and preferences, (including advance care planning and end of life planning if the consumer wishes)
Action 5.7.1: End-of-life care processes
- To identify and respond to a patient approaching end of life
- Support and respond to the changing needs of a patient in preparation of end of life
Action 5.7.2: End-of-life care support
Patient, family, carers and substitute decision-makers are supported to:
- a) Discuss advance care planning
- b) Review and develop documents that meet the patient's current needs and preferences
- c) Discuss aspects of requesting and declining of care or services (including responding to reversible acute conditions)
Action 5.7.3: End-of-life care planning
Using processes applied from comprehensice care to plan and deliver palliative care that:
- a) and b) Prioritises patient comfort, dignity, spiritual, cultural, and psychosocial needs
- c) Supports changes in pain and symtpoms are identified and managed
- d) Faciltitates access to medicines and equipemnt for pain and symptom management
- e) Communicates information about palliative care preferences
- f) Supports access to specialist palliative care where needed
- g) Faciliates a suitable environment for care
- h) Communicates information about loss and bereavement to family
Action 5.7.4: Implementing end-of-life processes
Processes in place in the last days of life to:
- a) Recognise and respond to a patient being in the last days of life and respond accordingly
- b) Manage pain symtpoms (including 24 hours access to relevant medications)
- c) Provide pressure, oral, eye, bowel, and bladder care
- d) Identify and respond to delirium
- e) Reduce the need for hospital transfers (if in line with patient preferences)
Strengthened Quality Standards framework analysis - Aged Care Quality Standards
Failure to comply with the requirements could lead to an organisation being penalised or reprimanded.
End-of-Life Care Skills Required for Healthcare Staff

For healthcare staff to be truly effective in end-of-life care, a comprehensive skill set is essential. Here are the expanded skills:
| Skill | Key Elements |
|---|---|
| Communication Skills |
The ability to converse openly about death, dying, and other sensitive subjects is crucial. Staff must also be adept at actively listening to patients and their families. |
| Emotional Intelligence |
Understanding and managing one's emotions and being able to perceive the emotions of the patient and family members is crucial. This also involves having empathy and providing emotional support when needed. |
| Technical Skills |
Expertise in managing physical symptoms, such as pain, nausea, or breathlessness, is imperative. This often involves pharmacological intervention, symptom assessment and relief measures. |
| Teamwork |
Effective collaboration within a multidisciplinary team, including nurses, doctors, social workers, and spiritual advisors, is essential for providing holistic care. |
| Ethical Skills |
Staff need to navigate complex ethical situations, respecting patient autonomy and providing dignified care, while balancing the needs and wishes of family members. |
How to Assess Staff Competency in End-of-Life Care
For a holistic assessment of staff competency in end-of-life care, a multi-faceted approach is needed:
- Direct Observations: Supervisors or experienced peers can observe staff as they interact with patients. Focus should be on communication, technical skills, and ethical decision-making.
- Simulated Scenarios: Staff can be tested in a simulated setting to assess both their technical and soft skills in end-of-life care.
- Self-assessments: Staff can be asked to rate their own end-of-life care skills and comfort levels, allowing for reflection and self-awareness.
- Feedback from Peers and Patients: Evaluations can be collected from colleagues and patients to gather diverse perspectives on a staff member's competency on end-of-life care.
Strategies to Support Healthcare Staff Improve End-of-Life Care Skills
Supporting employees in developing these crucial skills requires a long-term commitment in order to facilitate compliance to the standards and upholding a patient-centred approach to care:
Here are some potential strategies to support staff in end-of-life care skills development:
- Regular Training Workshops: Ongoing, in-house training sessions should be held to keep staff updated with the latest best practices.
- Mentoring Programs: Experienced staff can be paired with newer staff for one-on-one mentorship.
- Online Modules: Given the busy schedules of healthcare professionals, having online resources that can be accessed at their convenience is beneficial.
- Employee Assistance Programs: The emotional toll of providing end-of-life care is significant. Offering psychological support can help staff cope better emotionally.
Sample Training Plan for the End-of-Life Care Training Requirement
Using the below competency assessment on end-of-life care skills, we can tailor a training plan to target gaps in skills displayed by staff..
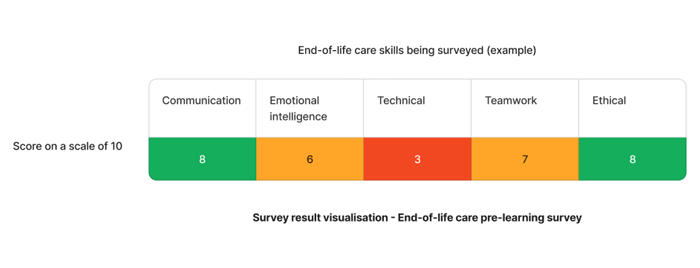
Based on the results - "technical" skills require actioning.
Need end-of-life care training for your organisation?
Contact Ausmed today and see how we can support with your end-of-life care requirements!
Staff Competency Assessment for End-of-Life Care - Example
The following is an example survey that learning and development coordinators and other educational managers may use to asses staff competency on end-of-life care.
Staff Survey - End-of-Life Care Competency
-
How comfortable are you discussing end-of-life choices with patients?
- 1. Not comfortable at all
- 2. Somewhat comfortable
- 3. Comfortable
- 4. Very comfortable
- 5. Extremely comfortable
-
Rate your ability to manage symptoms in end-of-life patients. (on a scale of 1-5)
- [Answer here]
-
How confident are you in working as part of a multidisciplinary team?
- 1. Not confident at all
- 2. Somewhat confident
- 3. Confident
- 4. Very confident
- 5. Extremely confident
-
Do you feel you can handle the emotional aspects of end-of-life care?
- 1. Yes
- 2. Somewhat
- 3. No
-
On a scale of 1-5, how well do you think you uphold the ethics of end-of-life care?
- [Answer here]
-
How prepared do you feel to provide culturally sensitive end-of-life care?
- 1. Not prepared at all
- 2. Somewhat prepared
- 3. Prepared
- 4. Very prepared
- 5. Extremely prepared
Conclusion
Providing quality end-of-life care is crucial and requires well-trained staff. Implementing a robust training program will equip healthcare professionals with the necessary skills to deliver compassionate, effective care.
References
- Australian Department of Health and Aged Care, 2019. 'What is Palliative Care?'
- Australian Commission on Safety and Quality in Health, 2015. 'National Consensus Statement: Essential elements for safe and high-quality end-of-life care'
- Australian Commission on Safety and Quality in Health, 2023. 'Comprehensive Care Standard'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.15'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.16'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.17'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.18'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.19'
- Australian Commission on Safety and Quality in Health, 2023. 'NSQHS Action 5.20'
- Aged Care Quality and Safety Commission, 2023. 'Aged Care Quality Standard - Ongoing Assessment - 2.3 (b)'
- Aged Care Quality and Safety Commission, 2023. 'Stronger Standards, Better Aged Care Program - 5.7.1-5.7.4'



