Sleep apnoea is not just snoring and disrupted sleep - it’s a serious medical condition.
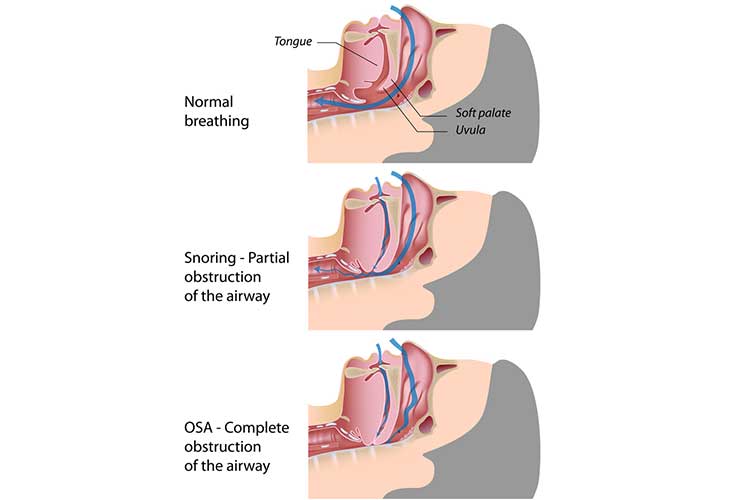
People who have obstructive sleep apnoea (OSA) will experience continuous episodes of partial or complete obstruction of the throat while sleeping (Sleep Health Foundation 2024a).
This obstruction occurs when the walls of the upper airway collapse and narrow, preventing air from reaching the lungs (Better Health Channel 2021).
A person with OSA stops breathing for a short period of time, typically 10 seconds to one minute (Better Health Channel 2021).
This cycle repeats multiple times during the night, leading to fragmented sleep, which causes a person to feel un-refreshed upon waking and experience daytime tiredness, poor concentration and general fatigue (Better Health Channel 2021).
How Sleep Apnoea Affects Breathing
Someone with sleep apnoea will:
- Cease breathing completely (apnoea), and/or
- Experience severely restricted breathing (hypopnoea).
(Better Health Channel 2021)
Note: Central sleep apnoea also causes breathing to stop and start during sleep, but it’s not the same as OSA. Rather than being caused by upper airway obstruction, central sleep apnoea occurs when there is disrupted communication between the brain and the muscles that control breathing (Mayo Clinic 2023; Newsom & Truong 2023).
While sleeping, a person with OSA may experience the following cycle between 5 to 30 times every hour:
- Muscles of the airway relax, a person’s breathing slows and snoring may begin.
- The airway is blocked, which causes breathing to stop.
- Oxygen in the blood decreases and the heart rate slows. The body struggles for air.
- The brain arouses and jolts the airway clear.
- The person gasps for air, possibly violently, disturbing their sleep.
- Breathing returns to normal.
- The cycle begins again.
(Mayo Clinic 2023)
How Prevalent is Sleep Apnoea?
An estimated 5% of Australians experience sleep apnoea. Around one in four men over the age of 30 years are affected (Better Health Channel 2021).
Causes of Sleep Apnoea
While any person can develop OSA, risk factors include:
- Obesity
- Being male
- Pregnancy
- Older age
- Alcohol consumption
- Smoking
- Certain conditions, including endocrine disorders (e.g. diabetes, hypothyroidism), neurological disorders (e.g. stroke, spinal cord injury) and Down syndrome
- Large tonsils and adenoids
- Taking certain medications, including sleeping tablets and sedatives
- Nasal congestion and/or obstruction
- Facial structure and muscle size.
(Better Health Channel 2021; Slowik et al. 2024)
Symptoms of Sleep Apnoea
- Snoring
- Tossing and turning in the night
- Gasping and choking in the night
- Daytime tiredness
- Reduced concentration
- Irritability and decreased mood
- Depression
- Anxiety
- Impotence and reduced sex drive
- Morning headaches
- Nocturia.
(Sleep Health Foundation 2024a; Better Health Channel 2021)

What are the Consequences of Sleep Apnoea?
Evidence indicates that people who have moderate to severe OSA will have other health problems. This includes a higher risk of heart attack, stroke, depression, hypertension and diabetes (Sleep Health Foundation 2024a).
Furthermore, people who have OSA are roughly two and a half times more prone to motor vehicle accidents than those without it due to inadequate sleep (Sleep Health Foundation 2024a).
Severity of Sleep Apnoea
- Normal sleep: Less than 5 breathing interruptions per hour
- Mild sleep apnoea: Between 5 and 15 breathing interruptions per hour
- Moderate sleep apnoea: Between 15 and 30 breathing interruptions per hour
- Severe sleep apnoea: Over 30 breathing interruptions per hour.
(Better Health Channel 2021)
Diagnosing Sleep Apnoea
If the symptoms of OSA are present, such as snoring, breathing pauses and sleepiness during the day, a person may want to be checked for OSA. This condition is typically diagnosed by an overnight sleep study (Sleep Health Foundation 2024a).
Treatment for Sleep Apnoea
It’s necessary to know the cause of a person’s sleep apnoea, as no single treatment is applicable for everyone (Sleep Health Foundation 2024b).
Lifestyle changes are considered to be the first line of treatment for sleep apnoea - specifically, losing weight and reducing alcohol consumption (Better Health Channel 2021).
In addition to lifestyle changes, it is often recommended that patients wear a mask at night to prevent their throats from collapsing. The mask gently transmits increased air pressure to the throat. The term for this is continuous positive airway pressure (CPAP). A person with OSA should work with a health professional to find the mask and machine that works for them (Better Health Channel 2021). CPAP is typically very successful at managing the symptoms and effects of OSA (Sleep Health Foundation 2024a).

A mouthguard or similar apparatus may be useful for people with mild to moderate sleep apnoea (Better Health Channel 2021).
In severe cases where other therapies have been unsuccessful, surgery to the palate and base of the tongue might be recommended. This surgery is best undertaken by otolaryngologists, who are specifically trained in sleep-related surgery (Better Health Channel 2021).
Test Your Knowledge
Question 1 of 3
Experiencing between 5 and 14 interruptions per hour is a sign of…?
Topics
References
- Better Health Channel 2021, Sleep Apnoea, Victoria State Government, viewed 14 November 2024, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/sleep-apnoea
- Mayo Clinic 2023, Central Sleep Apnea, Mayo Clinic, viewed 14 November 2024, https://www.mayoclinic.org/diseases-conditions/central-sleep-apnea/symptoms-causes/syc-20352109
- Newsom, R & Truong, K 2023, Central Sleep Apnea, Sleep Foundation, viewed 14 November 2024, https://www.sleepfoundation.org/sleep-apnea/central-sleep-apnea
- Sleep Health Foundation 2024a, Obstructive Sleep Apnea (OSA), Sleep Health Foundation, viewed 14 November 2024, https://www.sleephealthfoundation.org.au/sleep-disorders/obstructive-sleep-apnoea
- Sleep Health Foundation 2024b, Treatment Options for Obstructive Sleep Apnea (OSA), Sleep Health Foundation, viewed 14 November 2024, https://www.sleephealthfoundation.org.au/sleep-disorders/treatment-options-for-obstructive-sleep-apnoea-osa
- Slowik, JM, Sankari, A & Collen, JF 2024, ‘Obstructive Sleep Apnea’, StatPearls, viewed 14 November 2024, https://www.ncbi.nlm.nih.gov/books/NBK459252/
 New
New