Bowel cancer is the fourth most common and second most deadly cancer in Australia (Cancer Australia 2022).
Colonoscopies are crucial in the early recognition and treatment of bowel cancer and may lead to an increased chance of survival (ACSQHC 2020).
There are over 900,000 colonoscopies performed in Australia every year. The Colonoscopy Clinical Care Standard aims to ensure these procedures are performed safely and appropriately (ACSQHC 2020).
What is a Colonoscopy?
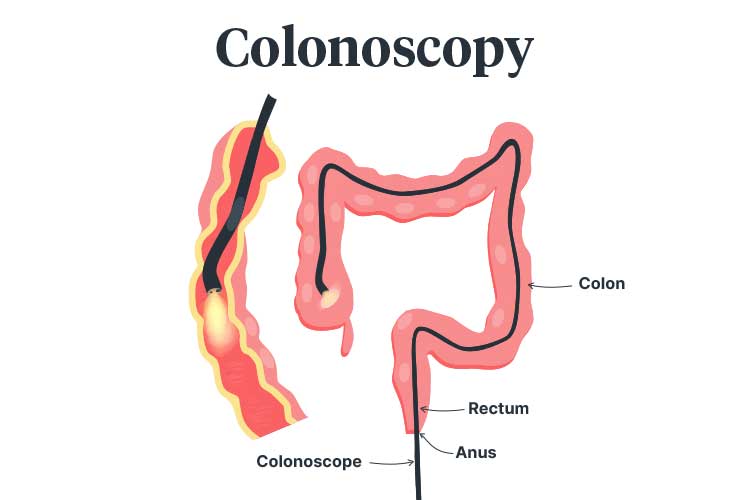
A colonoscopy is a diagnostic procedure wherein the inside of the colon (large bowel) is examined for signs of bowel cancer or illness (Healthdirect 2022).
It is performed using a flexible tube known as a colonoscope, which is inserted into the anus and guided through the colon. The colonoscope uses a camera and light to transmit a clear, magnified image of the colon lining to a monitor while it is being maneuvered (Better Health Channel 2023).
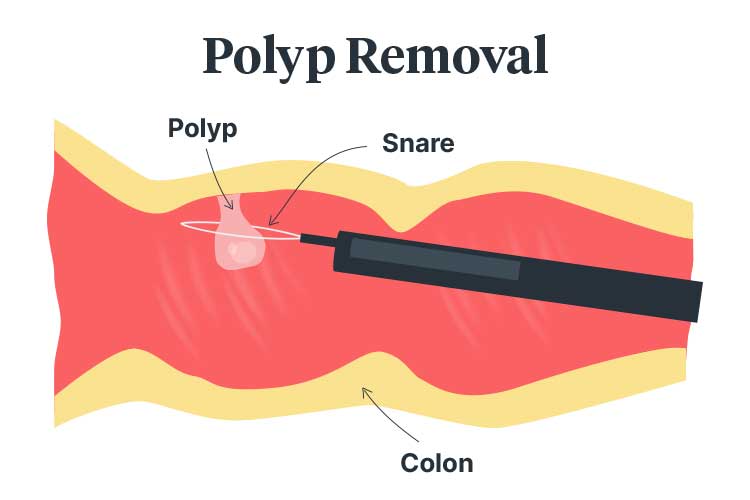
The clinician may need to remove polyps (potentially cancerous growths on the colon lining) or collect tissue samples during the procedure (ACSQHC 2020).
Why is a Colonoscopy Performed?
- To screen for bowel cancer
- To screen for polyps
- To determine the underlying cause of bowel-related symptoms.
(Better Health Channel 2023)
Who Should Undergo a Colonoscopy?
Generally, colonoscopies are indicated for patients who:
- Are experiencing bowel-related symptoms such as:
- Rectal bleeding
- Blood in stools
- Pus or mucus in stools
- Unexplained abdominal pain
- Changes in bowel habits (e.g. unexplained and prolonged diarrhoea)
- Have undergone a faecal occult blood test (FOBT) that came back positive (i.e. blood has been found)
- Are at high risk of bowel-related illness due to having chronic bowel disease, or a family history of bowel disease or bowel cancer
- Are experiencing unexplained weight loss
- Have been recommended to undergo a colonoscopy following a previous colonoscopy.
(Healthdirect 2022; Better Health Channel 2023; Cancer Council Victoria 2018)
Due to the potential harms of colonoscopies, the Royal Australian College of General Practitioners (2018) does not recommend colonoscopies for people who are only at average risk of bowel cancer. Instead, a FOBT is the preferred screening method for these people (Healthdirect 2022).
How is a Colonoscopy Performed?
Prior to the procedure, the patient will need to clear out their bowels. This is known as bowel preparation.
Bowel preparation may involve:
- Dietary changes a few days before the procedure. The patient should be given specific instructions detailing what they can and cannot consume
- Strong laxatives to cause diarrhoea
- Consuming clear fluids to prevent dehydration
- Changes to medicines.
(ACSQHC 2020; Healthdirect 2022)
Bowel preparation should only be directed by a medical practitioner or appropriately trained clinician. When changes to medicines are considered, the patient should be closely observed.
The procedure itself takes about 15 to 60 minutes. The patient is positioned onto their left side and sedated before the colonoscope is inserted. The colonoscope is guided to the terminal ileum (the end of the colon where it meets the small intestine), then slowly withdrawn so that the clinician can assess the colon lining. Throughout this process, air will be introduced in order to expand the colon for easier visualisation (Healthdirect 2022; Better Health Channel 2023; Robinson 2022).
If polyps are found, they will be removed and sent to pathology for further examination (ACSQHC 2020).
Following the procedure, the patient may experience:
- Abdominal bloating
- Gas and flatulence
- Abdominal cramping
- Rarely, blood in stools if a polyp or biopsy was taken.
(Better Health Channel 2023; Healthdirect 2022)
Potential Colonoscopy Complications
- Nausea, bloating, abdominal distension or chills caused by bowel preparation
- Dehydration (fever, dizziness or severe headache) or electrolyte imbalance caused by bowel preparation
- Allergic reaction to laxatives
- Cardiovascular events caused by sedation
- Infection
- Colonic perforations
- Bleeding.
(Healthdirect 2022; RACGP 2018)
Colonoscopy Clinical Care Standard
In 2020, the Australia Commission on Safety and Quality in Health Care released the Colonoscopy Clinical Care Standard. This standard aims to ensure that colonoscopies are safe, appropriate and beneficial when performed (ACSQHC 2020).
The standard contains nine quality statements:
1. Initial Assessment and Referral
A healthcare professional referring patients for colonoscopies should provide a comprehensive referral. This will allow receiving clinicians to assess whether a colonoscopy is appropriate for each patient.
The referral should include:
- Reasons for referral, including the patient’s symptoms and a preliminary diagnosis
- Relevant medical and family history, including history of cancers and genetic predispositions
- Comorbidities
- Current medicines
- Previous relevant treatment
- Results of previous investigations (e.g. FOBT, previous colonoscopies).
Colonoscopy appointments should be allocated based on patients’ clinical needs.
(ACSQHC 2020)
2. Appropriate and Timely Colonoscopy
Patients should be assessed for colonoscopy suitability using national evidence-based guidelines and colonic disease epidemiology. Clinicians should take into account:
- Likely benefits of the procedure
- Potential risks of the procedure
- Potential risks of not undergoing the procedure.
(ACSQHC 2020)
3. Informed Decision-making and Consent
Patients should be provided with clear, comprehensive information about the procedure detailing:
- Bowel preparation
- Sedation
- The procedure itself
- Reasons for the procedure
- Likely benefits of the procedure
- Potential risks of the procedure
- Potential risks of not undergoing the procedure
- Out-of-pocket costs
- Alternative options.
Patients must give informed consent prior to the procedure.
(ACSQHC 2020)
4. Bowel Preparation
Bowel preparation should be prescribed to patients based on:
- Individual risk factors
- Comorbidities
- Current medicines
- Their previous experiences with bowel-cleansing medicines.
Ensure patients understand the purpose of bowel preparation, how and when to use it and what the potential side effects are. Patients should also be advised of any required medicine changes they need to make while undergoing bowel preparation.
It is recommended that patients use a split-dose regimen (where consumption of the bowel preparation is split between the night before the procedure and the morning of the procedure).
(ACSQHC 2020)
5. Sedation
Patients should be sedated before the colonoscopy. In order to identify any potential risks associated with sedation (such as cardiovascular, respiratory or airway compromise), the clinician should assess the patient’s:
- General health
- Comorbidities
- Medicines
- Previous experiences with sedation or anaesthesia.
If any risks are identified, patients should be supervised by an anaesthetist or another appropriately trained practitioner during the procedure.
(ACSQHC 2020)
6. Clinicians
Sedation and colonoscopies must be performed by appropriately qualified clinicians with the required credentials.
(ACSQHC 2020)
7. Procedure

When performing a colonoscopy:
- Allow enough time for mucosal inspection
- If the patient has undergone a bowel resection, thoroughly assess the remaining bowel
- Document the procedure thoroughly
- Retrieve all polyps that have been removed and send them for a histopathology examination
- Ensure histology samples generated through the National Bowel Cancer Screening Program are identified
- Record any procedural complications
- Inform patients about any procedural complications and how they have been managed.
(ACSQHC 2020)
8. Discharge
Prior to discharge, patients should be informed about:
- What happened during the procedure
- Whether the procedure was performed satisfactorily
- Preliminary results
- Whether polyps or biopsies were taken
- Whether any procedural complications occurred
- Any required follow-ups
- When they will receive the final results.
(ACSQHC 2020)
Once meeting discharge criteria, patients should be discharged into the care of a responsible adult with discharge instructions detailing postoperative care and when to resume regular activities (ACSQHC 2020).
Immediately following the procedure, patients should generally refrain from:
- Driving
- Travelling alone on public transport
- Operating machinery
- Signing legal documents
- Consuming alcohol.
(Healthdirect 2022)
Patients should also be advised on what to do if they experience postoperative complications such as:
- Severe bloating or abdominal pain
- Persistent nausea and vomiting
- Black, tar-like stools
- Persistent anal bleeding
- Fever or chills.
(Healthdirect 2022)
9. Reporting and Follow-Up
Patients should be provided with the results of the procedure, along with any follow-up recommendations. If prompt intervention or treatment is required, arrangements should be made and communicated.
Test Your Knowledge
Question 1 of 3
How should patients be positioned during a colonoscopy?
Topics
References
- Australian Commission on Safety and Quality in Health Care 2020, Colonoscopy Clinical Care Standard, Australian Government, viewed 16 February 2024, https://www.safetyandquality.gov.au/publications-and-resources/resource-library/colonoscopy-clinical-care-standard-revised-2020
- Better Health Channel 2023, Colonoscopy, Victoria State Government, viewed 16 February 2024, https://www.betterhealth.vic.gov.au/health/ConditionsAndTreatments/colonoscopy
- Cancer Australia 2022, Cancer in Australia Statistics, Australian Government, viewed 16 February 2024, https://www.canceraustralia.gov.au/impacted-cancer/what-cancer/cancer-australia-statistics
- Cancer Council Victoria 2018, Faecal Occult Blood Test (FOBT): A Test for the Early Signs of Bowel Cancer, Cancer Council Victoria, viewed 16 February 2024, https://www.cancervic.org.au/downloads/cpc/bowel/fobt_info_sheet.pdf
- Healthdirect 2022, Colonoscopy, Australian Government, viewed 16 February 2024, https://www.healthdirect.gov.au/colonoscopy
- Royal Australian College of General Practitioners 2018, ‘Early Detection of Cancers: Colorectal Cancer’, Guidelines for Preventive Activities in General Practice, 9th edn, viewed 16 February 2024, https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/guidelines-for-preventive-activities-in-general-pr/early-detection-of-cancers/colorectal-cancer
- Robinson, J 2022, Colonoscopy, WebMD, viewed 16 February 2024, https://www.webmd.com/colorectal-cancer/colonoscopy-what-you-need-to-know
 New
New