In Australia, over 700,000 people have sustained a brain injury that restricts their normal daily activities to some extent (Brain Injury Australia 2023).
Among those with brain injuries, three-quarters are under 65 years of age, and two-thirds acquired their brain injury before the age of 25 (Brain Injury Australia 2023).
What is an Acquired Brain Injury?
The umbrella term acquired brain injury (ABI) refers to any type of brain injury that occurs following birth (Queensland Health 2022). It may be the result of:
- Trauma
- Stroke
- Brain tumour
- Poisoning
- Infection or disease
- Near drowning or another episode of reduced oxygen supply
- Substance use disorder.
(Queensland Health 2022)
Every person with an ABI is different. Long-term effects may range from mild to severe, depending on the patient (Better Health Channel 2014).
What is a Traumatic Brain Injury?
A traumatic brain injury (TBI) is a type of ABI that occurs following an impact to the head, causing damage to the brain tissue (Better Health Channel 2014).
These head injuries can be classified as either:
- Non-penetrating injuries (closed head injuries), where an external force moves the brain inside the skull (e.g. sports injury)
- Penetrating injuries, where an object has impacted the head and pierced through the skull (e.g. bullet injury).
(NINDS 2023)
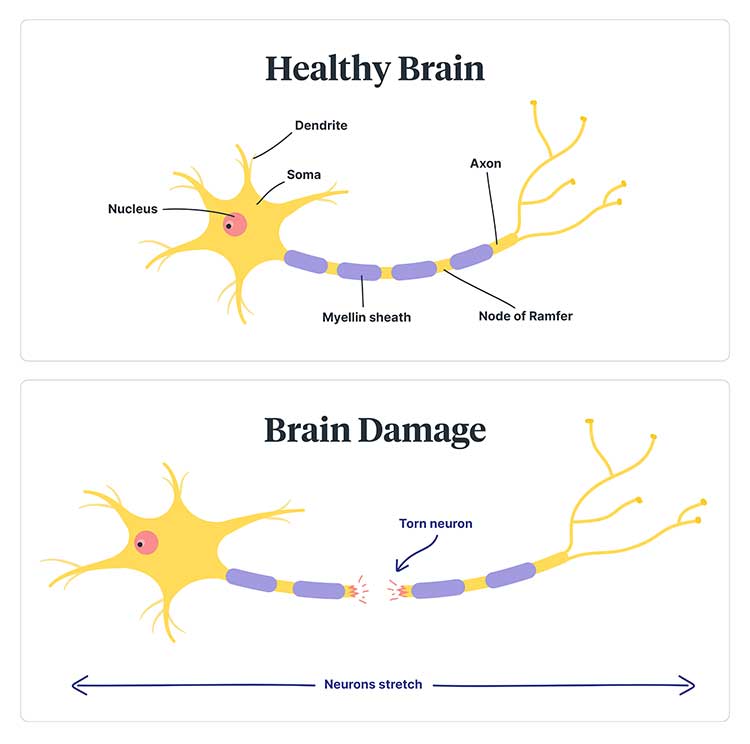
As a result of the head being forced to move rapidly, the brain can tear, stretch, or become bruised or swollen. Force can also cause oxygen starvation and bleeding in the brain (Synapse 2021).
Common signs and symptoms of a TBI immediately following the injury include loss of consciousness, which can last from minutes to days, and post-traumatic amnesia, which also varies in length (Mayo Clinic 2021; Headway 2019a).
Other symptoms include nausea and vomiting, seizures, confusion and headaches (Mayo Clinic 2021).
Consequences of a Traumatic Brain Injury
There are many consequences following a TBI, not only for the patient but also for their family and friends. Relationships, social networks and the person’s lifestyle may be affected and ultimately changed forever. The patient and their family may experience difficulties as they navigate these changes and grieve for their losses (Better Health Channel 2014).
Common problems associated with TBIs include:
- Emotional changes, such as agitation, anxiety and depression
- Behavioural changes
- Problems with autonomic system regulation resulting in hypertension, hypotension, tachycardia and temperature regulation abnormalities
- Cardiovascular system problems, including arrhythmias and deep vein thrombosis
- Cognitive deficits such as impaired memory, learning, reasoning, judgement and attention
- Sleep disturbances
- Nausea and vomiting
- Genitourinary system problems, including incontinence and neurogenic bladder
- Neurological system dysfunction such as seizures, sensory deficits, neglect and lack of spatial awareness
- Neuromuscular system problems, including rigidity, contractures, tremors and spasticity
- Post-concussive symptoms
- Respiratory complications
- Skin integrity problems from lack of mobility and moisture.
(Mayo Clinic 2021; Kishner 2023; Chen et al. 2017; Headway 2019b; Physiopedia 2019a)
Recovery Following a Traumatic Brain Injury
Recovery depends on the extent and location of the brain damage, the age and general health of the person, and what treatment they have had directly following the injury and during their rehabilitation (Better Health Channel 2014).
A person with an ABI may experience long-term changes including:
- Medical difficulties
- Changes in physical and sensory abilities
- Changes in cognition
- Psychological and behavioral changes
- Communication difficulties.
(Queensland Health 2022)
Nursing Care of a Patient with a Traumatic Brain Injury
The life expectancy of someone with a TBI is generally shorter compared to the general population. Those who have retained independent mobility tend to live longer (Physiopedia 2019).
Each patient with a TBI will display different symptoms, so nursing interventions and considerations should be individualized to each patient.
Often, these interventions will include strategies for:
- Managing physical impairments
- Behavior management
- Communication management
- Emotional support
- Environmental management (safety of their environment and home preparation)
- Family support
- Health education
- Memory training
- Socialization enhancement
- Speech therapy
- Any unilateral neglect management.
(Mauk 2012)
As you can see, the patient with a TBI may have very complex needs. Therefore, it is extremely important to adopt an interprofessional approach to treatment.
Family members also need to be involved in their loved one’s treatment. They will need to support the patient during this process and may also need to support themselves during their loved one’s recovery. Nurses need to ensure that family members:
- Are adequately informed about TBIs and their effects
- Respect that recovery may be slow
- Understand that difficulties may arise during the recovery process.
(Better Health Channel 2014)
Topics
References
- Better Health Channel 2014, Acquired Brain Injury, Victoria State Government, viewed 23 November 2023, https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/acquired-brain-injury
- Brain Injury Australia 2023, About Brain Injury, Brain Injury Australia, viewed 23 November 2023, https://www.braininjuryaustralia.org.au/
- Chen, Z et al. 2017, ‘Brain–Heart Interaction’, Circulation Research, vol. 121, no. 4, viewed 23 November 2023, https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.117.311170
- Headway 2019b, Continence Problems After Brain Injury, Headway, viewed 23 November 2023, https://www.headway.org.uk/media/7819/continence-problems-after-brain-injury-factsheet.pdf
- Headway 2019a, Post-traumatic Amnesia, Headway, viewed 23 November 2023, https://www.headway.org.uk/media/7915/post-traumatic-amnesia-factsheet-2019.pdf
- Kishner, S 2023, Post Head Injury Autonomic Complications, Medscape, viewed 23 November 2023, https://emedicine.medscape.com/article/325994-overview
- Mauk, K L 2012, Rehabilitation Nursing: A Contemporary Approach to Practice, Jones & Bartlett Learning, Burlington, MA.
- Mayo Clinic 2021, Traumatic Brain Injury, Mayo Clinic, viewed 23 November 2023, https://www.mayoclinic.org/diseases-conditions/traumatic-brain-injury/symptoms-causes/syc-20378557
- National Institute of Neurological Disorders and Stroke 2023, Traumatic Brain Injury (TBI), U.S. Department of Health and Human Services, viewed 23 November 2023, https://www.ninds.nih.gov/health-information/disorders/traumatic-brain-injury-tbi
- Physiopedia 2019b, Healthy Aging with Traumatic Brain Injury, Physiopedia, viewed 23 November 2023, https://www.physio-pedia.com/Healthy_Aging_with_Traumatic_Brain_Injury
- Physiopedia 2019a, Medical Complications in Traumatic Brain Injury, Physiopedia, viewed 23 November 2023, https://www.physio-pedia.com/Medical_Complications_in_Traumatic_Brain_Injury
- Queensland Health 2023, What is Acquired Brain Injury (ABI), Queensland Government, viewed 23 November 2023, https://www.health.qld.gov.au/abios/asp/what_is_abi
- Synapse 2021, Traumatic Brain Injury, Synapse, viewed 23 November 2023, https://synapse.org.au/fact-sheet/traumatic-brain-injury/
 New
New 
